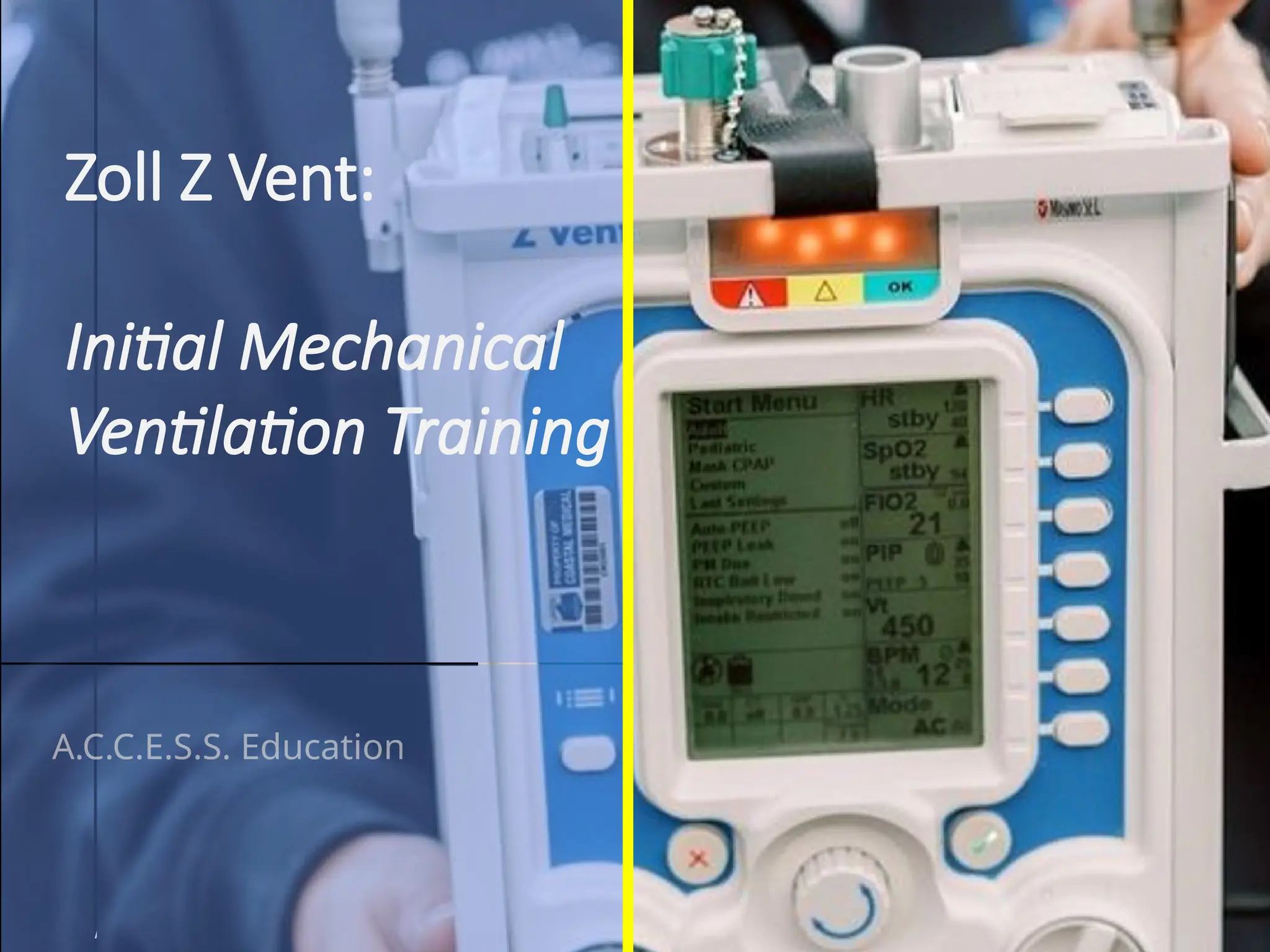
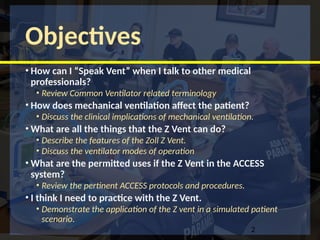
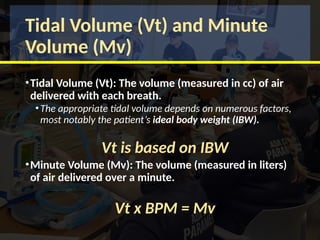
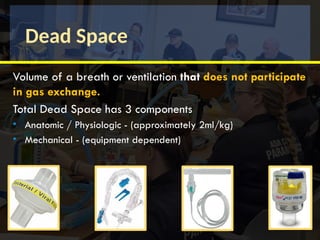
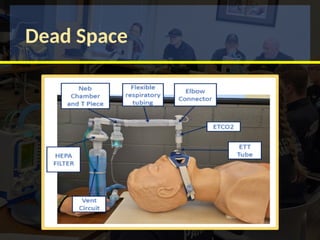
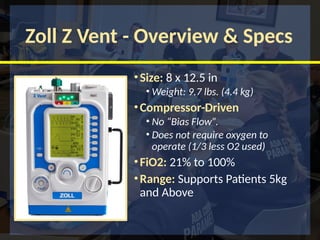
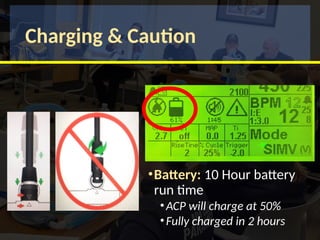
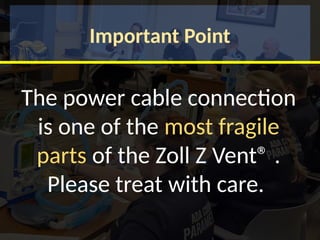
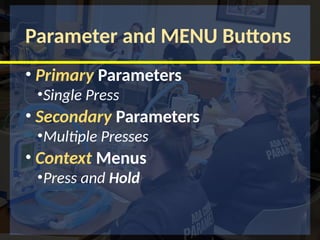
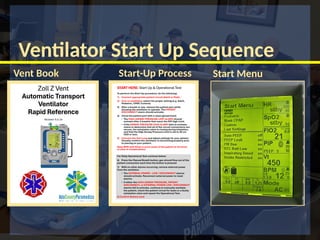
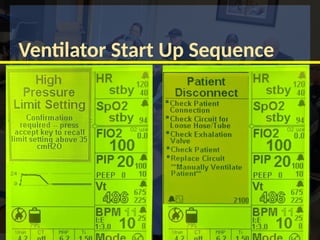
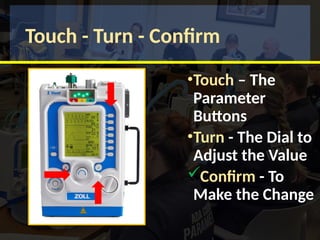
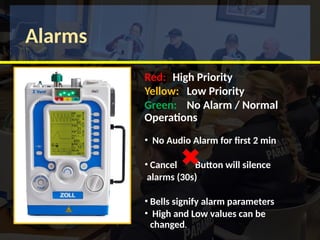
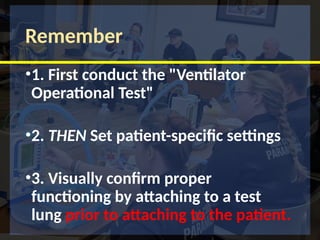
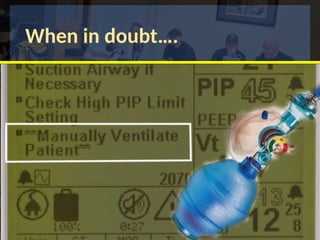
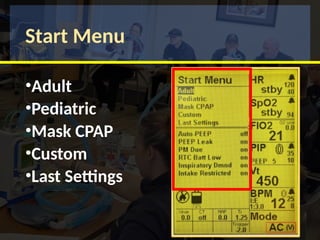
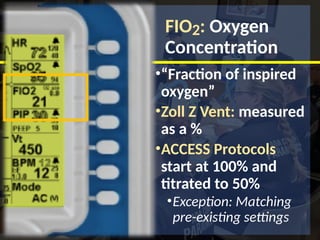
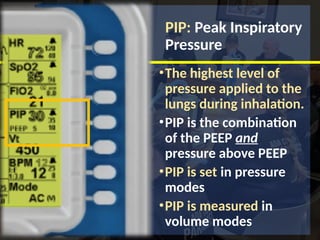
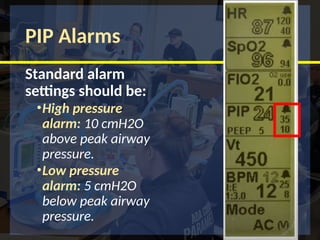
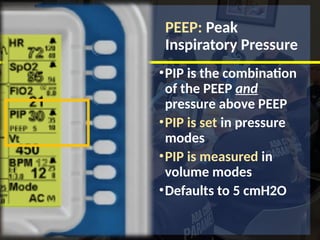
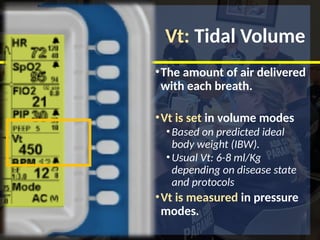
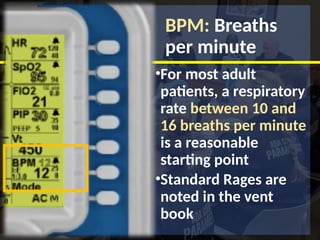
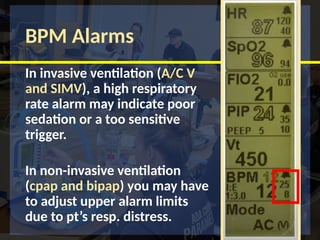
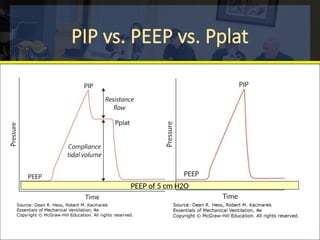
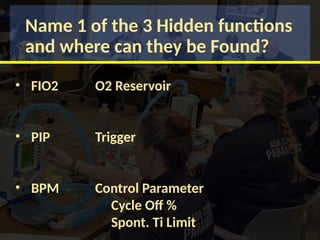
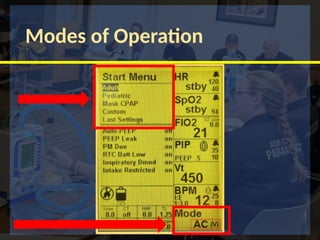
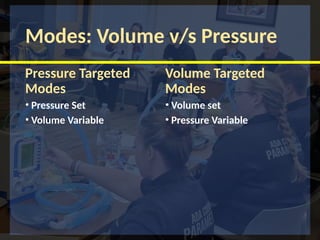
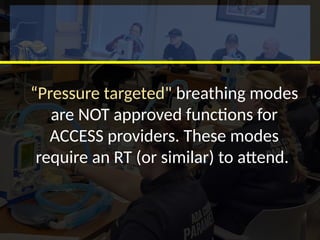
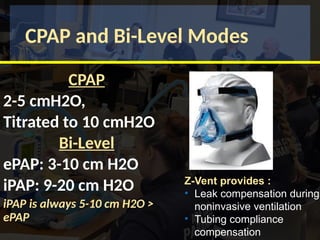
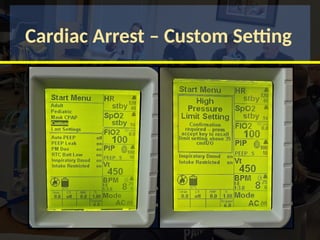
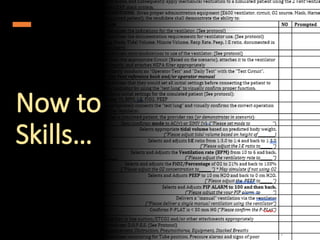
The document provides training objectives and essential information on the Zoll Z Vent mechanical ventilator, covering its functionality, terminology, and operation modes. It includes details on the clinical implications of mechanical ventilation, features of the Z Vent, and specific protocols for its use, emphasizing patient care and safety. Additionally, it outlines various settings, parameters, and scenarios to practice using the device effectively.