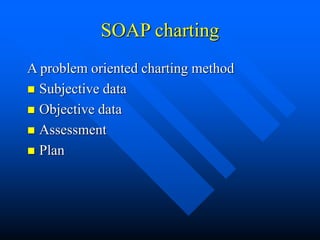
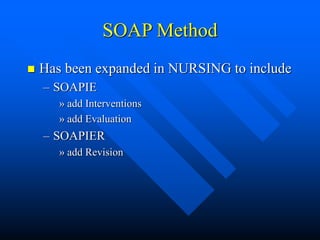
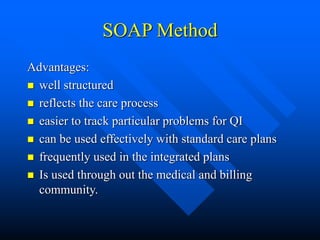
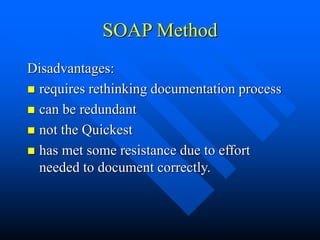
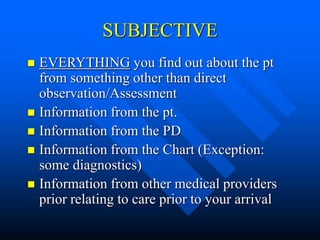
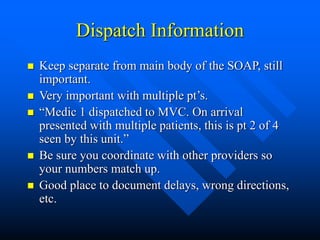
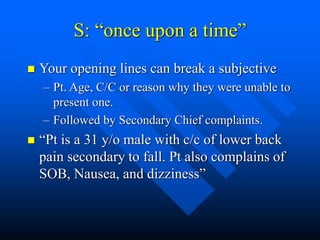
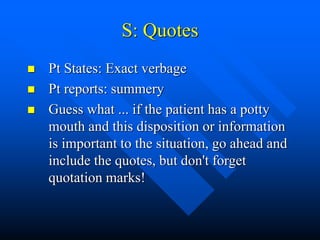
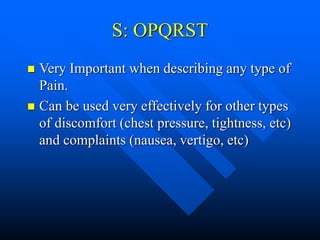
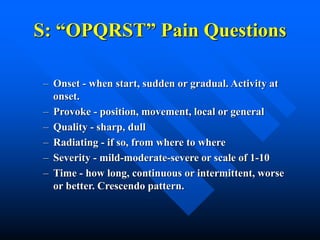
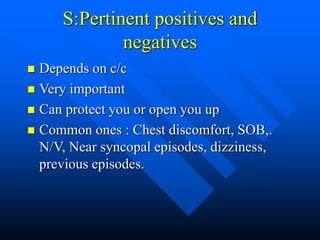
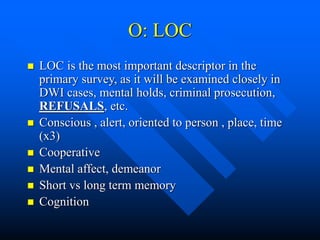
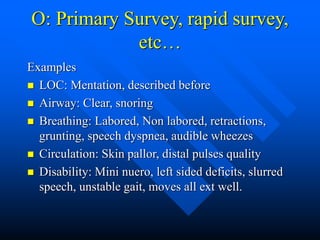
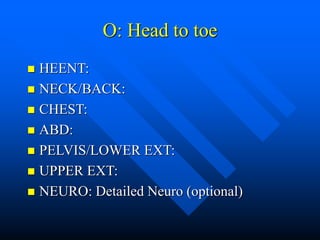
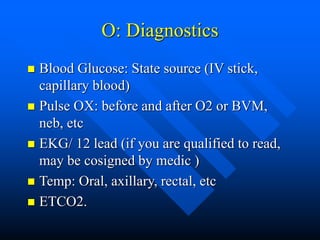
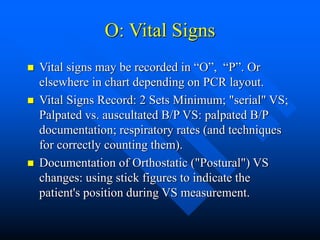
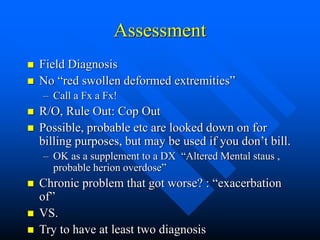
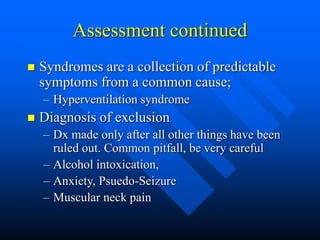
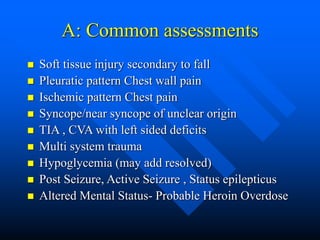
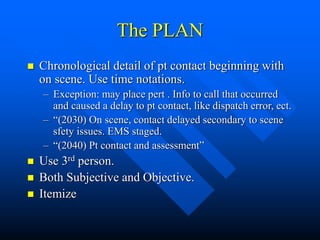
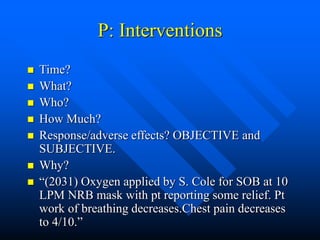
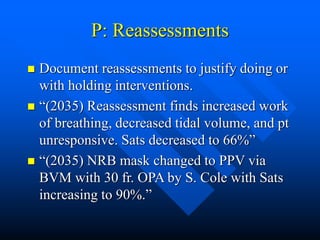
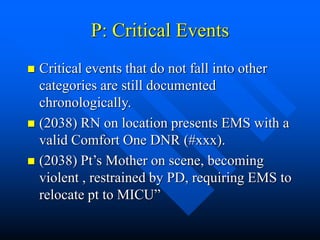
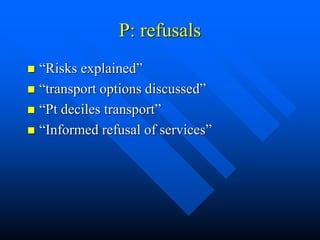
This document provides guidance on effective medical documentation using the SOAP note format. It discusses the goals of documentation, including writing consistently, comprehensively, and in a legally defensible manner. It then covers the components of the SOAP note format, with subjective (S) covering patient-reported information, objective (O) focusing on clinical observations, assessment (A) stating the patient's conditions, and plan (P) outlining treatment. The document emphasizes writing objectively and avoiding judgment.