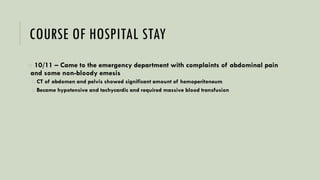
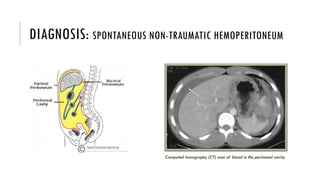
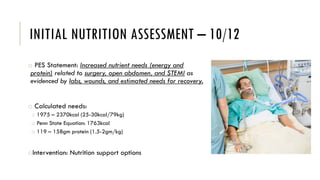
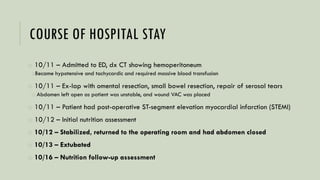
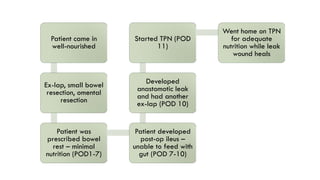
1) A 65-year-old man presented with spontaneous hemoperitoneum and required multiple surgeries including small bowel resection.
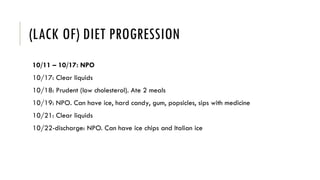
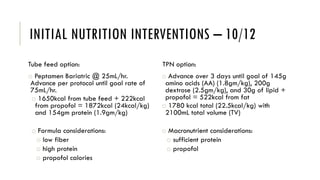
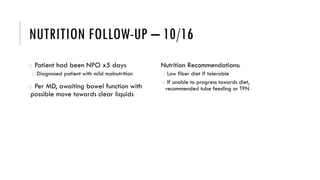
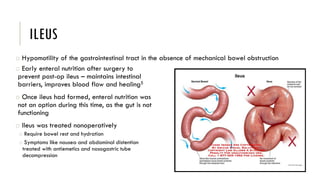
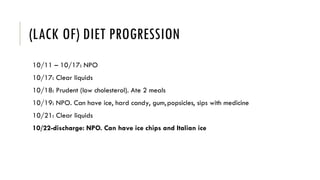
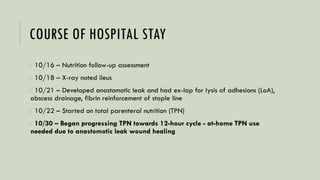
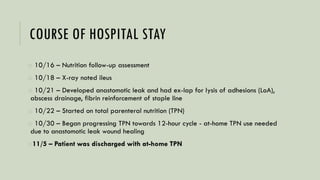
2) He developed complications including an ileus, myocardial infarction, and anastomotic leak, preventing enteral nutrition.
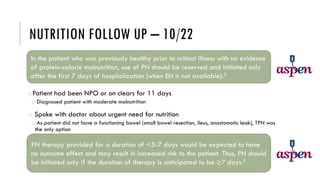
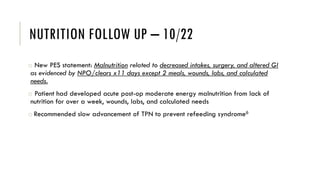
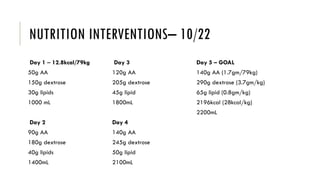
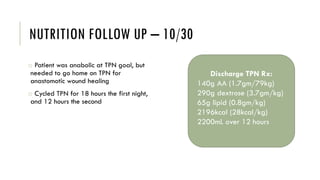
3) After 11 days without adequate nutrition, the patient was started on total parenteral nutrition (TPN) which was advanced cautiously due to his risk for refeeding syndrome.
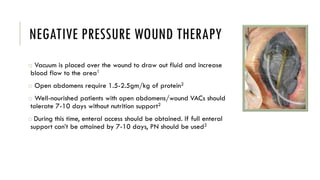
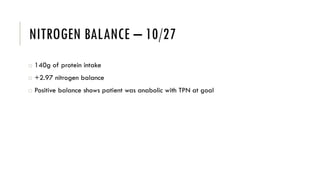
4) TPN met his nutritional needs and supported wound healing and recovery.