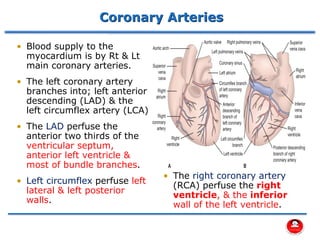
The document discusses coronary artery anatomy and acute myocardial infarction. It describes:
- The main coronary arteries that supply the heart and the regions each artery perfuses.
- How atherosclerosis leads to plaque buildup in arteries, reducing blood flow to the heart.
- How a plaque rupture can cause a clot that fully occludes a coronary artery, causing cell death in the myocardial region supplied by that artery - known as a myocardial infarction.















































![• Severe uncontrolled hypertension on presentation (blood
pressure >180/110 mm Hg)
• History of prior ischemic stroke greater than 3 months
• Known intracranial pathology not covered in contraindications
• Current use of anticoagulants in therapeutic doses
(international normalized ratio [INR] ≥2:3); known
bleeding diathesis
• Recent (within 2–4 weeks) internal bleeding
• Head trauma or traumatic or prolonged (>10 minutes)
• (CPR) or major surgery (<3 weeks)
• Pregnancy/ Dementia/ Active peptic ulcer
Relative Contraindications to Fibrinolytic
Therapy](https://image.slidesharecdn.com/14-acutemyocardialinfarction-230308183912-430f748b/85/14-Acute-Myocardial-Infarction-pdf-49-320.jpg)









