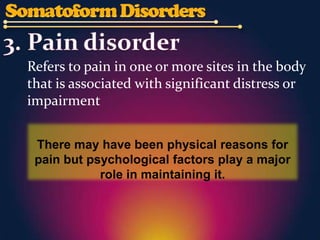
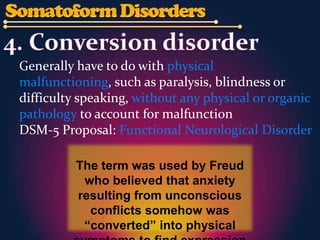
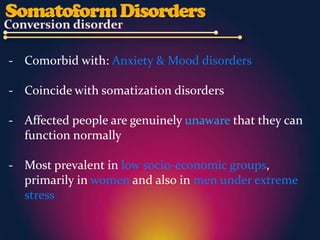
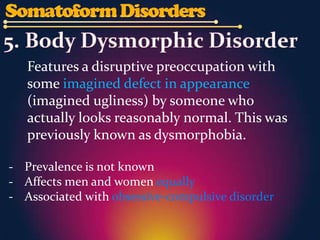
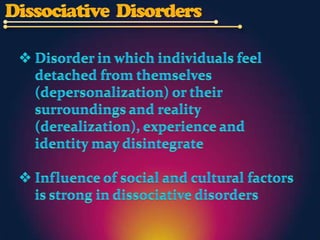
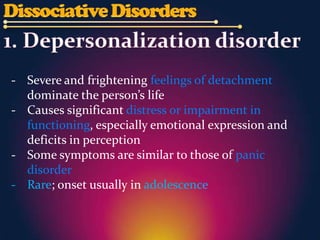
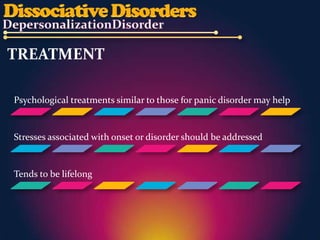
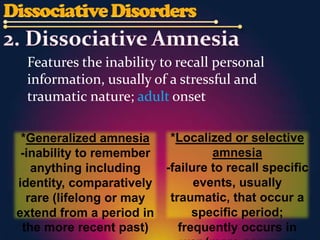
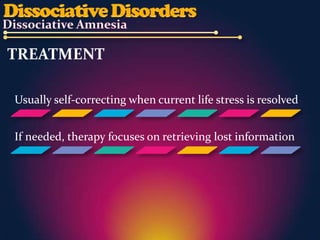
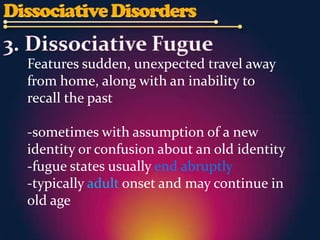
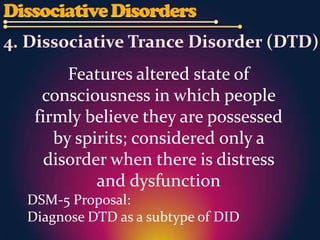
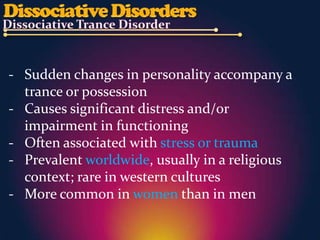
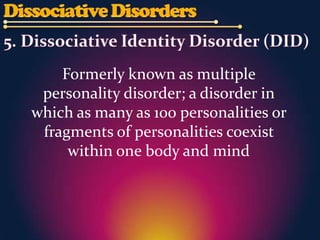
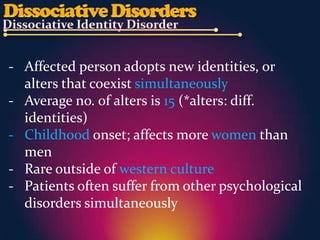
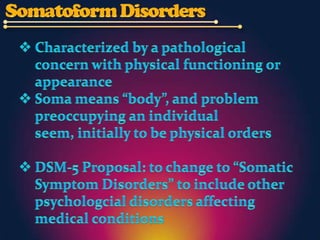
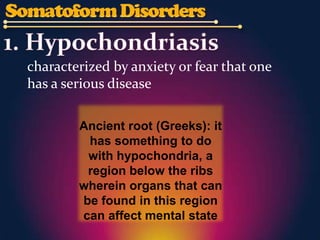
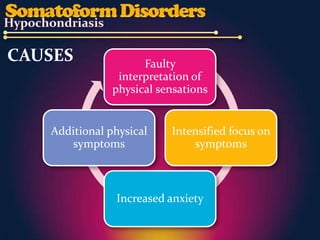
The document discusses several culture-bound syndromes and psychological disorders including hypochondriasis, somatization disorder, body dysmorphic disorder, dissociative identity disorder, and possession trance disorder. Many of these conditions involve physical or imagined symptoms that have psychological or cultural causes and can be treated with therapies like cognitive behavioral therapy.


![CULTURE-SPECIFIC SYNDROMES THAT FIT WITH
HYPOCHONDRIASIS
• Koro: belief, accompanied by severe anxiety and sometimes
panic, that the genitals are retracting into the abdomen
[mostly Chinese males]
• Dhat: associated w/ vague mix of physical
symptoms, including dizziness, weakness and fatigue that are
not so specific](https://image.slidesharecdn.com/somatoformdissociativedisordersfinal-120915084421-phpapp02/85/Somatoform-dissociative-disorders-5-320.jpg)

![Formerly known as Briquet’s syndrome [for
more than 100 yrs] and was changed in
1980 to somatization disorder
- Reports of multiple physical symptoms without
medical basis
- Runs in families (probable heritable basis)
- Rare (most prevalent among unmarried women
low in socioeconomic groups)
- Onset usually in adolescence; often persists into
old age](https://image.slidesharecdn.com/somatoformdissociativedisordersfinal-120915084421-phpapp02/85/Somatoform-dissociative-disorders-8-320.jpg)