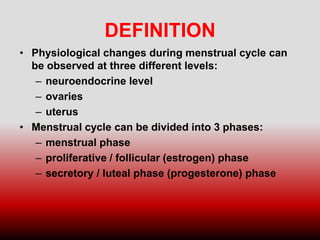
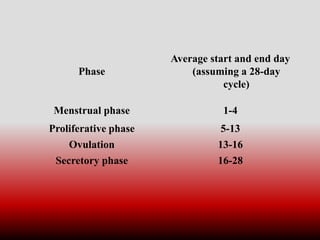
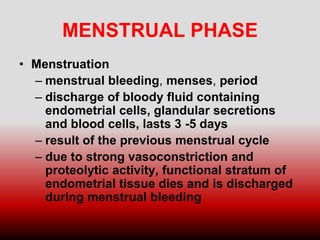
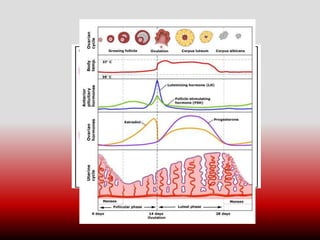
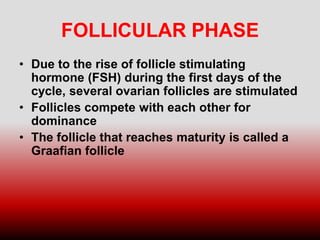
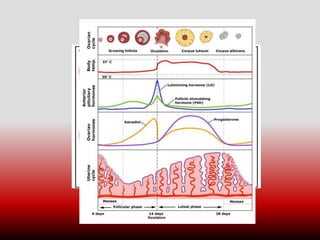
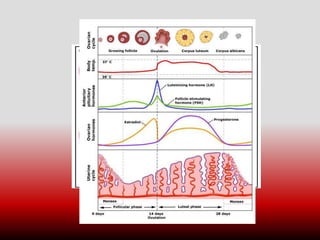
The menstrual cycle is the series of changes that occur in a woman's reproductive system in preparation for pregnancy. It is controlled by hormones and typically lasts around 28 days, though the length can vary. The cycle involves three phases - the menstrual, proliferative, and secretory phases. During ovulation, an egg is released from the ovaries if pregnancy does not occur. The cycle then repeats each month until menopause, which usually occurs between ages 45-55.