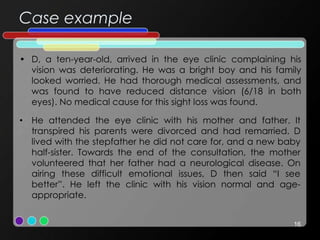
D, a 10-year-old boy, presented with deteriorating vision but no medical cause was found. During the consultation, it was revealed he lived with a stepfather he did not like and had family relationship issues. After discussing his difficult family situation, D reported that his vision had returned to normal. This suggests he may have been experiencing a somatoform disorder where psychological or emotional factors were affecting his physical symptoms.
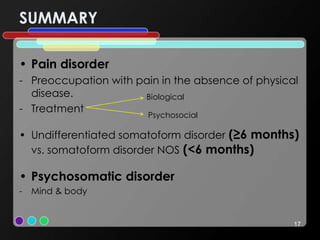
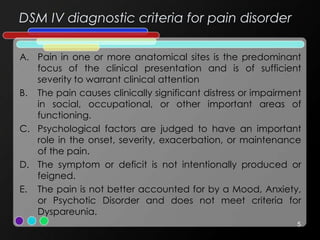
![PAIN DISORDER
• Definition:
Preoccupation with pain in the absence of
physical disease. The pain doesn’t follow a
neuroanatomic distribution. [1]
• Epidemiology:
1 month prevalence is 0.15-1.26%, >Female [2]
3](https://image.slidesharecdn.com/psyseminarsomatopsychosomato-140806002103-phpapp01/85/Somatoform-disorder-psychosomatic-disorder-3-320.jpg)
![PSYCHOSOMATIC DISORDER
Definition
Prevalence
Classification
Diagnosis
Etiology
Treatment
9
1. Psychological
factor medical
condition
2. Physical illness
emotional/ mental
disorder
Psyche (mind)
& Soma (body)
12.5% [3]](https://image.slidesharecdn.com/psyseminarsomatopsychosomato-140806002103-phpapp01/85/Somatoform-disorder-psychosomatic-disorder-9-320.jpg)