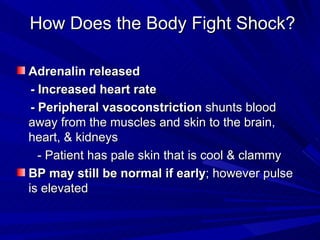
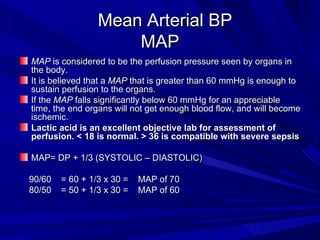
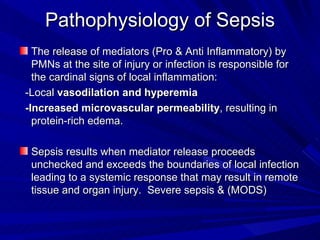
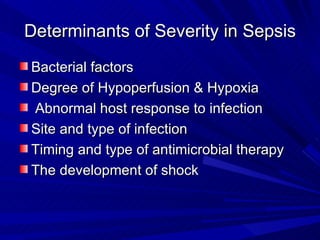
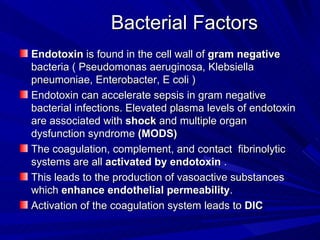
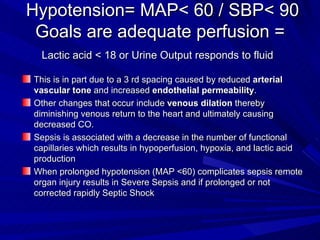
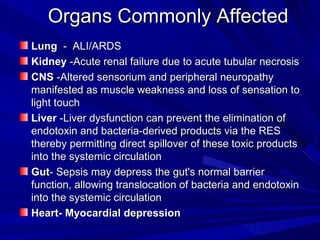
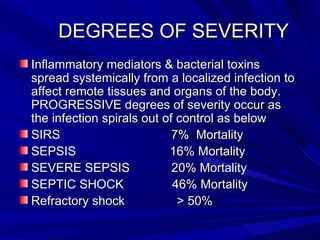
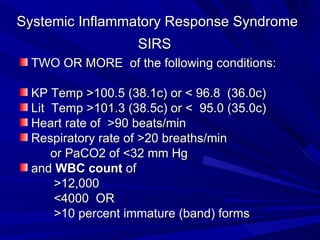
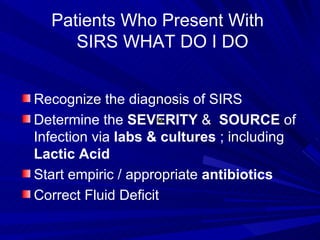
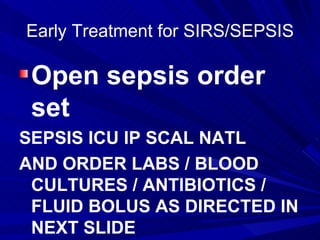
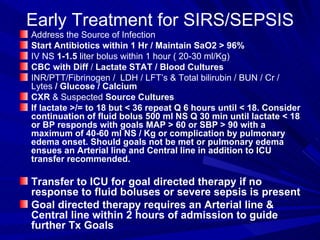
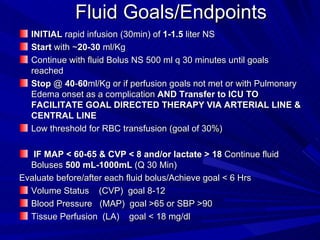
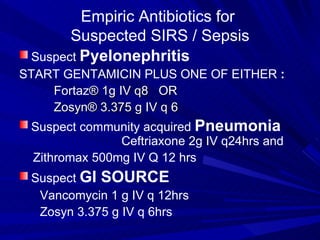
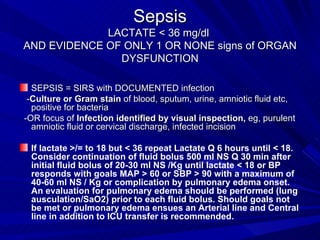
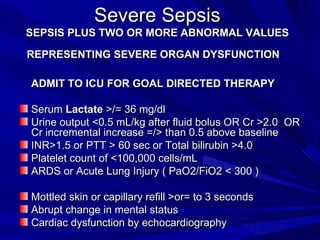
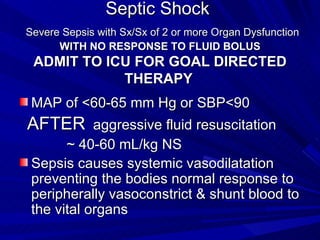
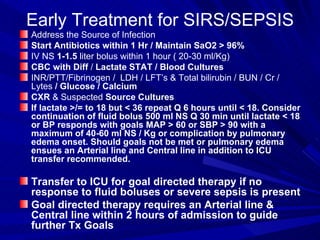
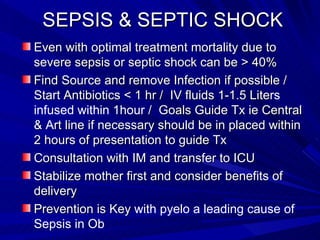
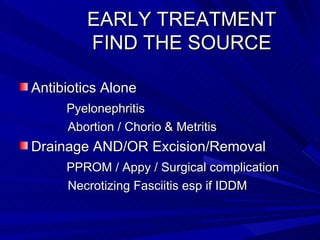
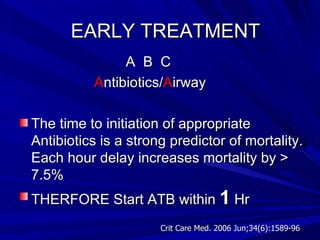
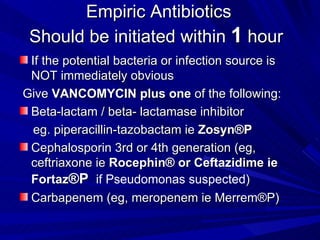
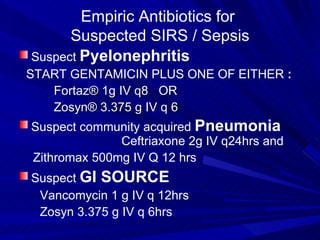
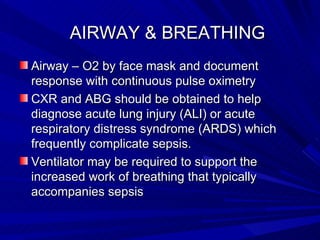
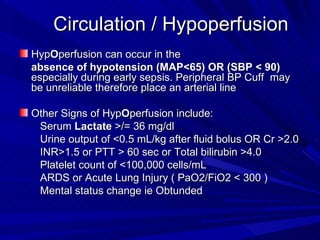
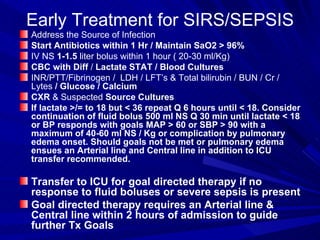
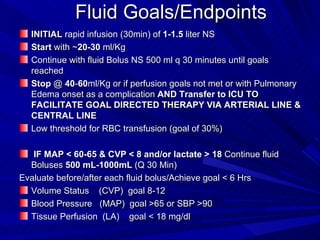
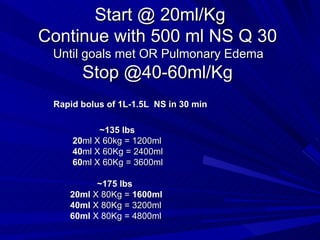
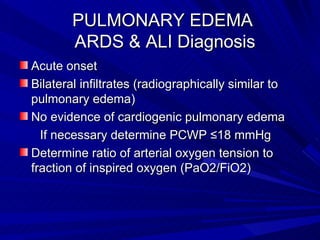
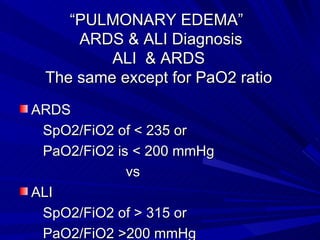
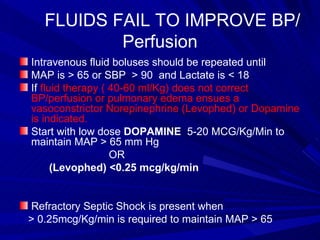
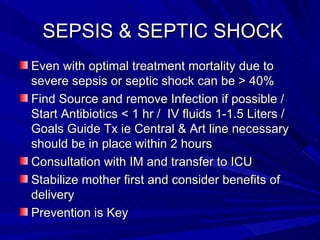
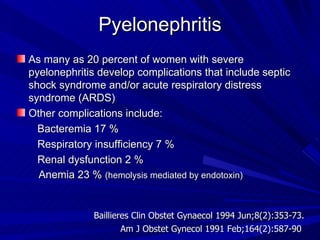
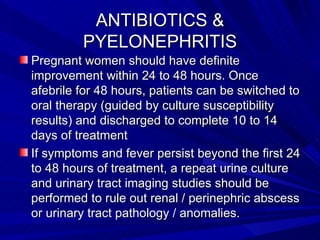
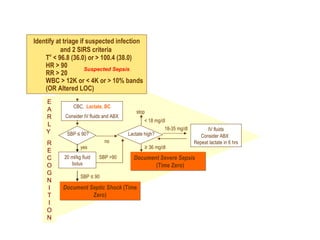
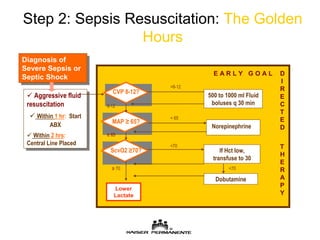
This document summarizes the pathophysiology, diagnosis, and initial management of sepsis and septic shock. It describes the progression from systemic inflammation to shock and multiple organ dysfunction. Early goals of treatment include identifying the infection source, administering antibiotics within 1 hour, providing intravenous fluid boluses, and monitoring lactate levels and perfusion targets. Patients with sepsis may progress to severe sepsis or septic shock, indicated by worsening organ dysfunction and hypotension not responding to fluids, requiring intensive care management and goals-directed therapy.