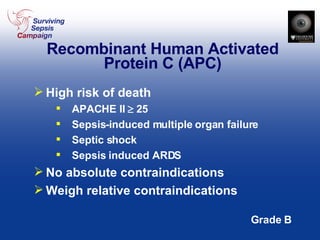
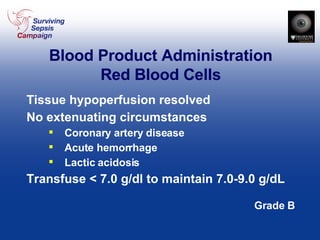
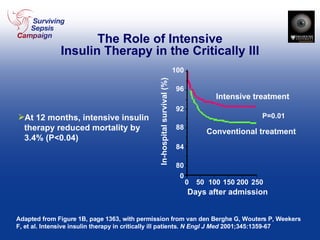
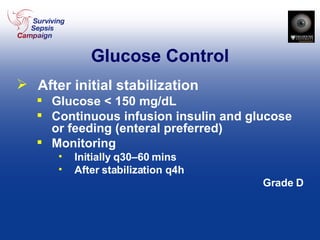
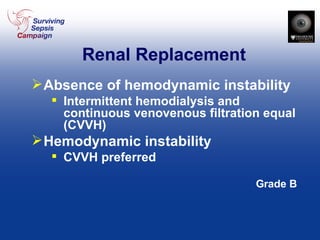
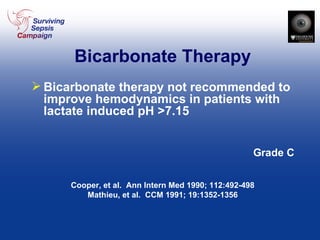
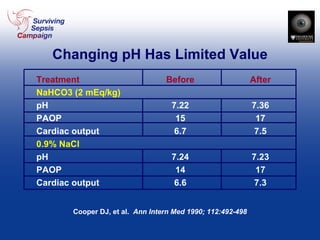
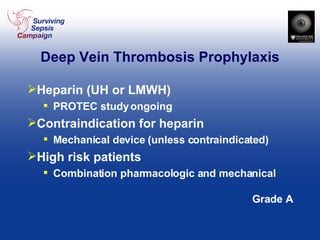
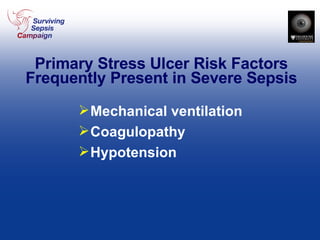
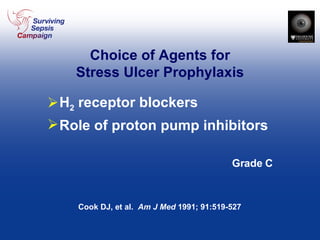
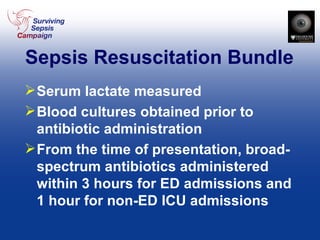
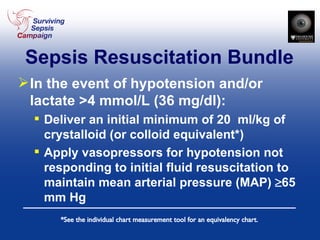
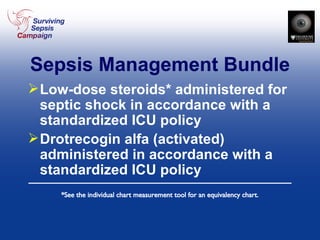
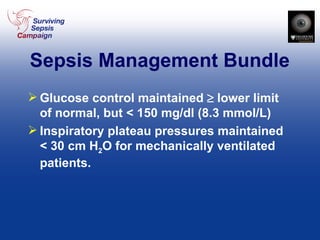
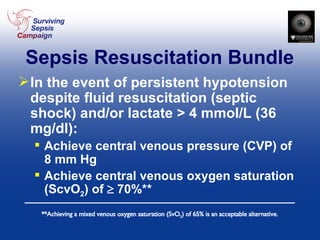
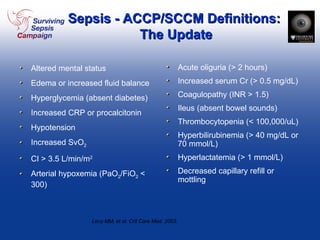
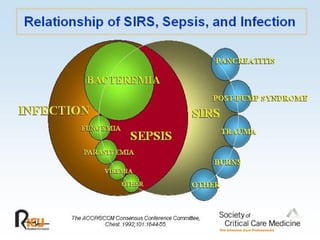
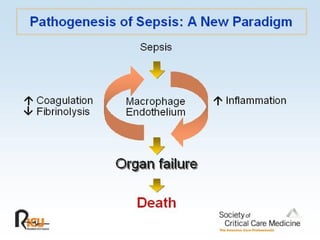
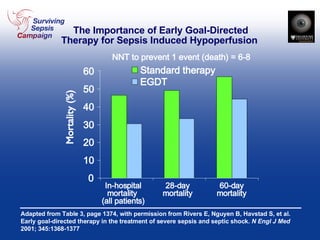
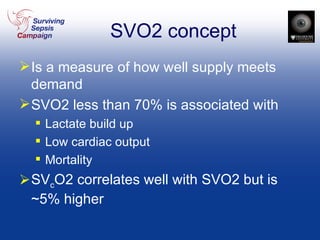
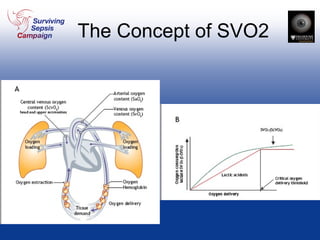
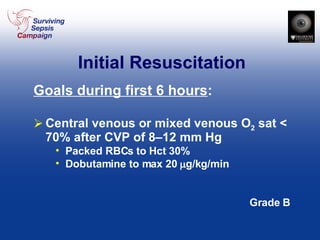
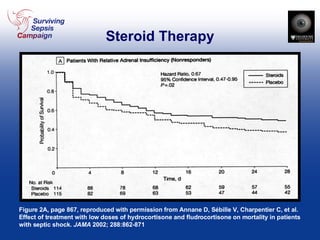
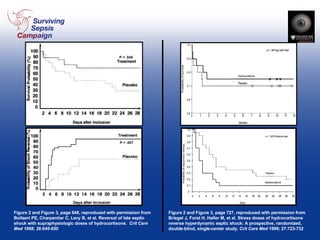
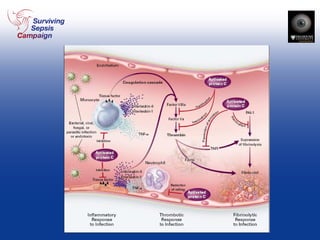
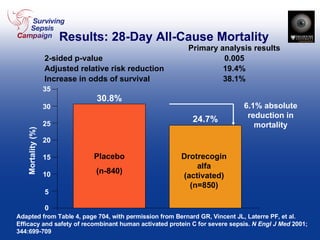
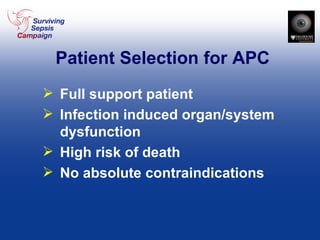
This document provides guidelines for the management of severe sepsis and septic shock. It discusses definitions of sepsis, systemic inflammatory response syndrome, and septic shock. It outlines initial resuscitation goals including fluid resuscitation, vasopressors, inotropic therapy, and goals for central venous pressure, mean arterial pressure, urine output, and central venous or mixed venous oxygen saturation. It provides recommendations on antibiotic therapy, source control, steroids, activated protein C, transfusion thresholds, glucose control, renal replacement therapy, stress ulcer prophylaxis, and implementing a sepsis resuscitation bundle.

![Initial Resuscitation Goals during first 6 hours : Central venous pressure: 8–12 mm Hg Mean arterial pressure 65 mm Hg Urine output 0.5 mL kg -1 /hr -1 Central venous (superior vena cava) or mixed venous oxygen [SvO 2 ] saturation 70% Grade B](https://image.slidesharecdn.com/sepsis-1204661418275516-4/85/Sepsis-14-320.jpg)


![Mortality and APACHE II Quartile Adapted from Figure 2, page S90, with permission from Bernard GR. Drotrecogin alfa (activated) (recombinant human activated protein C) for the treatment of severe sepsis. Crit Care Med 2003; 31[Suppl.]:S85-S90 APACHE II Quartile *Numbers above bars indicate total deaths Mortality (percent) 26:33 57:49 58:48 118:80](https://image.slidesharecdn.com/sepsis-1204661418275516-4/85/Sepsis-50-320.jpg)
![Mortality and Numbers of Organs Failing Adapted from Figure 4, page S91, with permission from Bernard GR. Drotrecogin alfa (activated) (recombinant human activated protein C) for the treatment of severe sepsis. Crit Care Med 2003; 31[Suppl.]:S85-S90 Percent Mortality 0 10 20 30 40 50 60 1 2 3 4 5 Placebo Drotrecogin Number of Organs Failing at Entry](https://image.slidesharecdn.com/sepsis-1204661418275516-4/85/Sepsis-51-320.jpg)