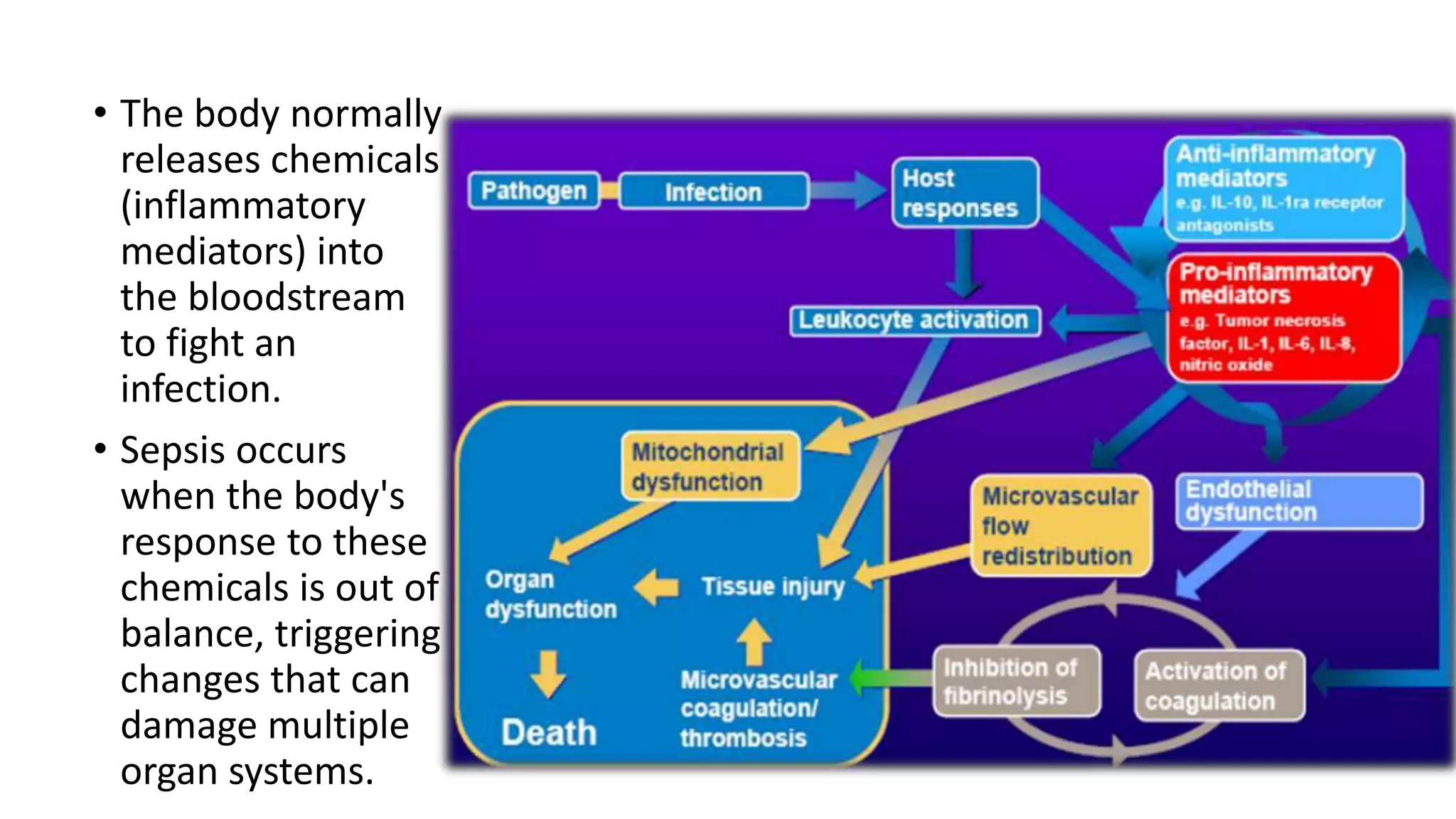
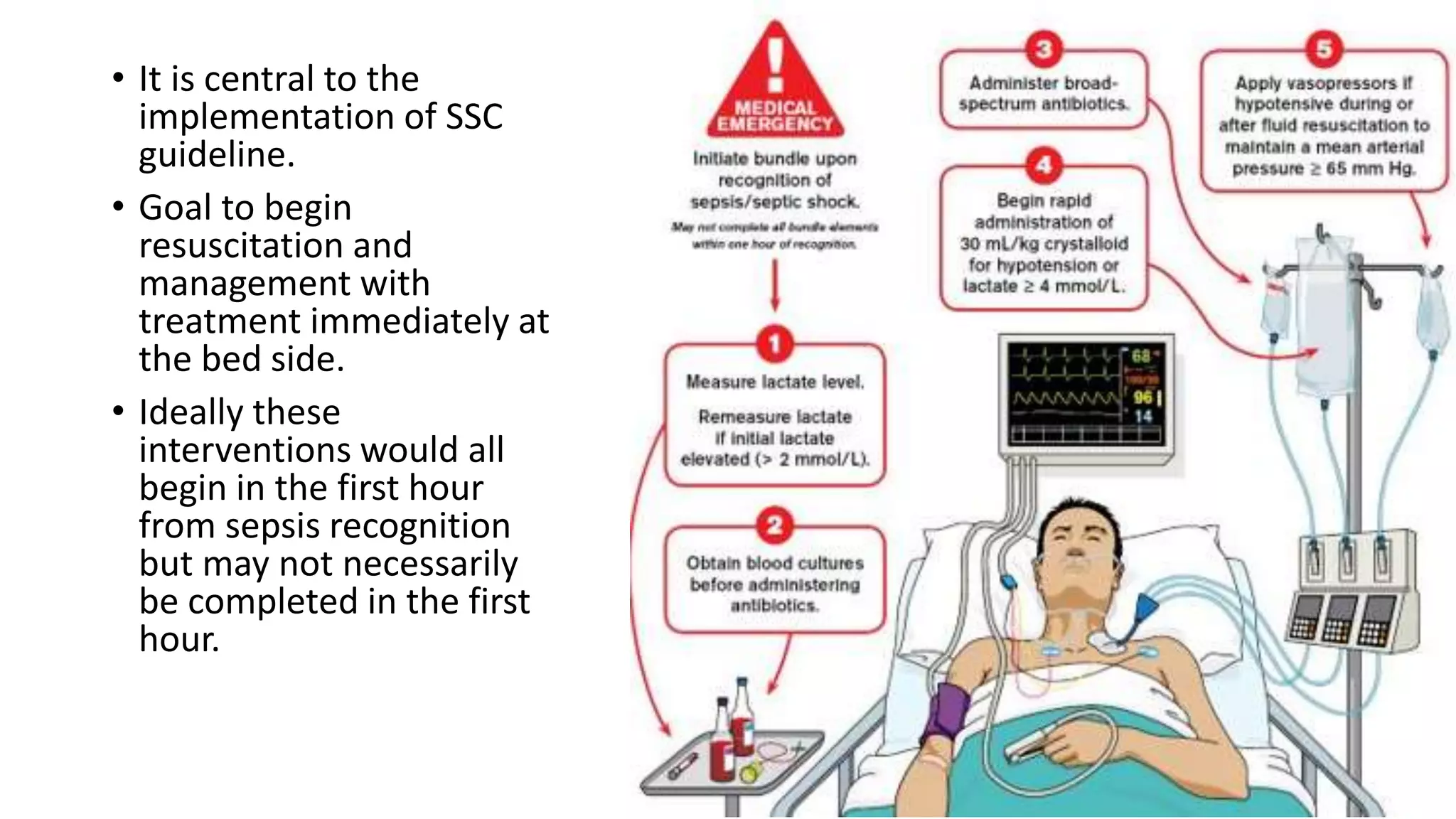
Sepsis and septic shock result from a dysregulated host response to infection that leads to organ dysfunction. Management involves immediate resuscitation within 1 hour with IV fluids, antibiotics, and vasopressors if needed. Ongoing care includes source control, frequent reassessment of volume status, and supportive care such as mechanical ventilation and nutrition. The goals are to treat the underlying infection while supporting failing organs until the host response normalizes. Sepsis affects millions worldwide and requires swift treatment to prevent progression to septic shock and death.









![Sequential [Sepsis-Related] Organ Failure
Assessment Score (SOFA)](https://image.slidesharecdn.com/sepsisandsepticshockpptfinal-190329022629/75/Sepsis-and-septic-shock-13-2048.jpg)
















![Blood transfusion
• If hemoglobin levels fall below 7 g/dL,
• Red blood cell transfusion is recommended to a target hemoglobin range
of 7-9 g/dL.
• Even in the absence of apparent bleeding platelet is transfused if platelet
counts fall below 10,000/µL
• DIC should first be ruled out with fibrinogen split products and peripheral
smears.
• Platelet transfusion may also be considered when bleeding risk is increased
and platelet counts are below 20,000/µl.
• Patients who are to undergo surgery or other invasive procedures may
require higher platelet counts (eg, ≥50,000/µL]).](https://image.slidesharecdn.com/sepsisandsepticshockpptfinal-190329022629/75/Sepsis-and-septic-shock-34-2048.jpg)


![References
• Available at:
http://www.survivingsepsis.org/guidelines/Pages/default.aspx. Accessed
June 24, 2016.
• emedicine.com. Accessed February 26, 2019].
• Rhodes A, Evans LE, Alhazzani W, et al. Surviving Sepsis Campaign:
International Guidelines for Management of Sepsis and Septic Shock: 2016.
Intensive Care Med. 2017;
• Singer M, Deutschman CS, Seymour CW, et al. The Third International
Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA.
2016;315(8):801-10.
• Howell MD, Davis AM. Management of Sepsis and Septic Shock. JAMA.
2017;](https://image.slidesharecdn.com/sepsisandsepticshockpptfinal-190329022629/75/Sepsis-and-septic-shock-41-2048.jpg)
