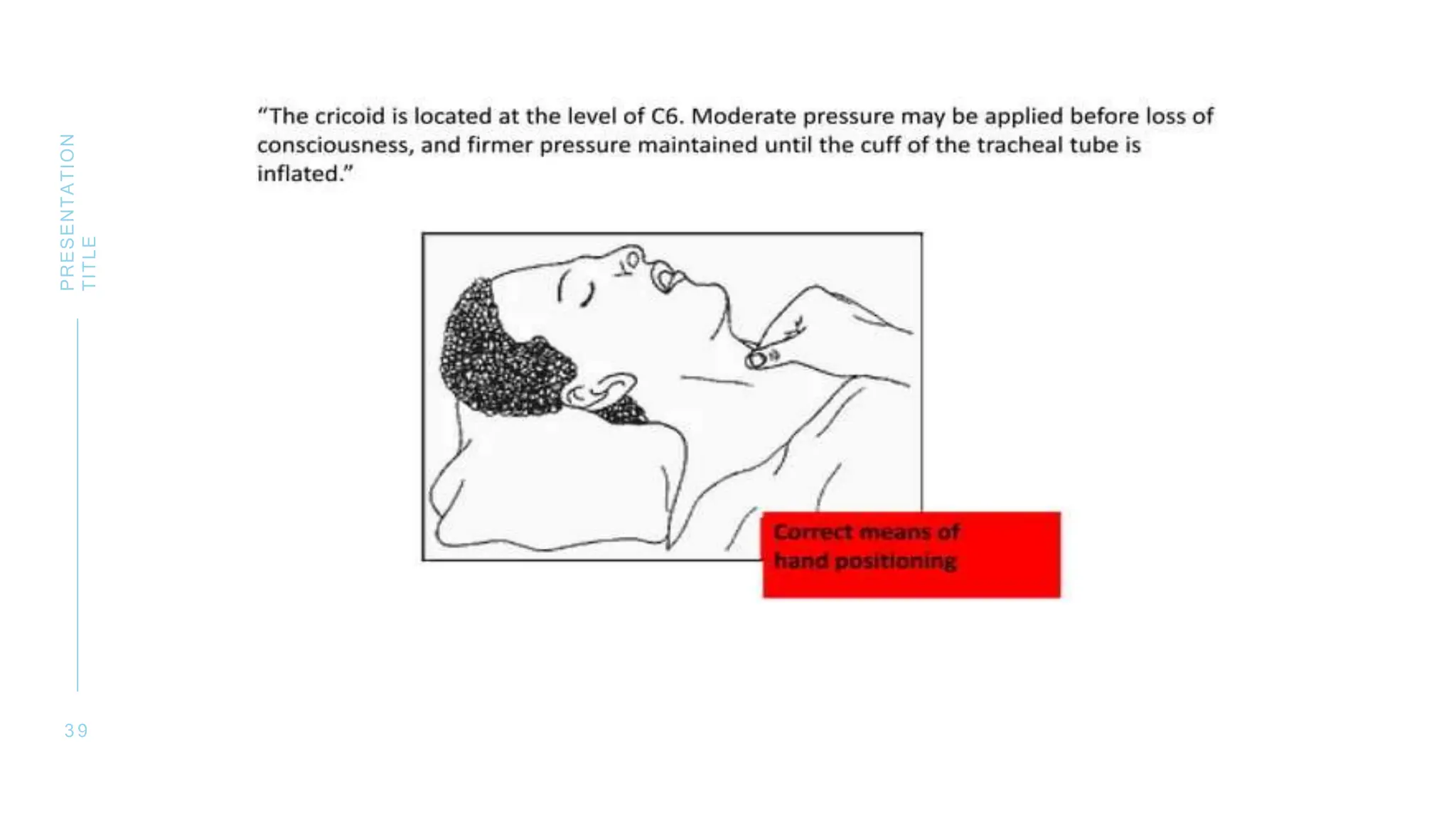
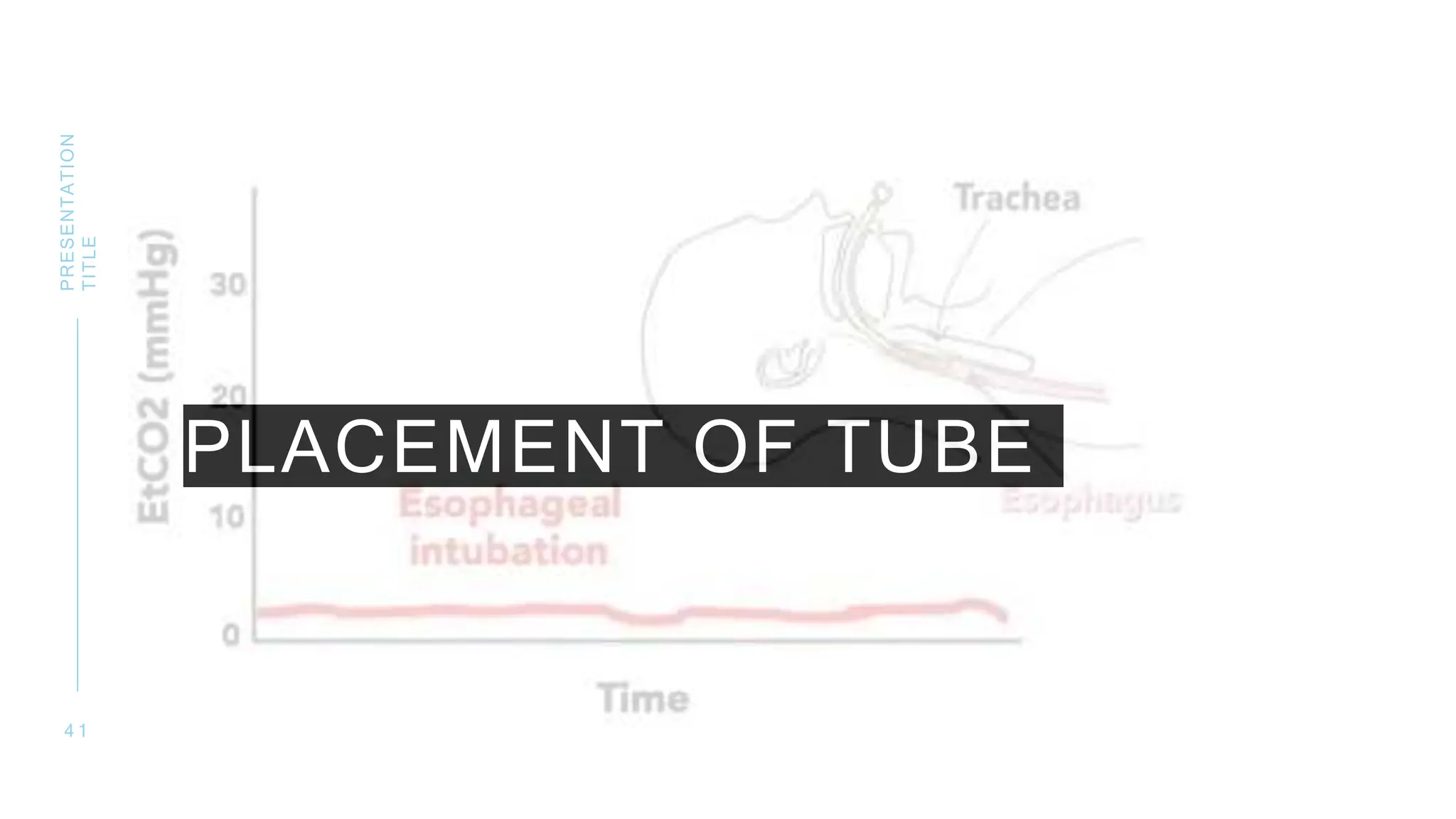
The document discusses Rapid Sequence Induction and Intubation (RSII), a procedure developed to minimize pulmonary aspiration risks during airway management. It outlines the history, preparation, techniques, and considerations for performing RSII, while identifying high-risk patient factors and discussing various pharmacological agents used. Additionally, it addresses potential complications, modern adaptations, and future directions for the procedure.