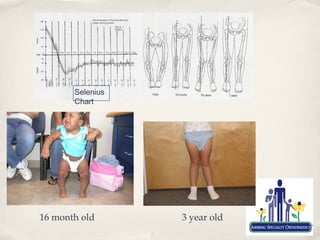
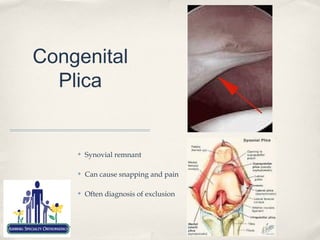
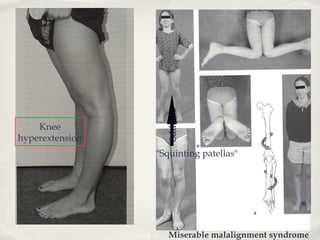
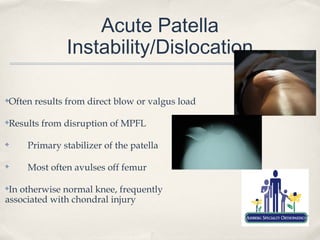
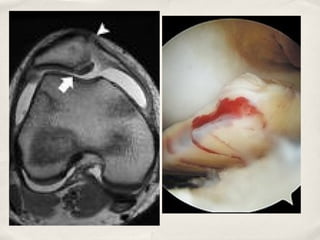
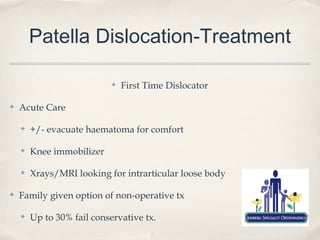
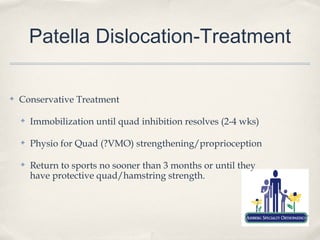
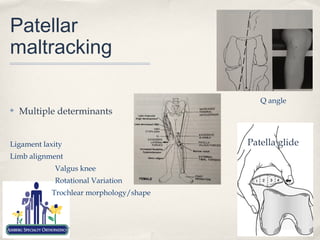
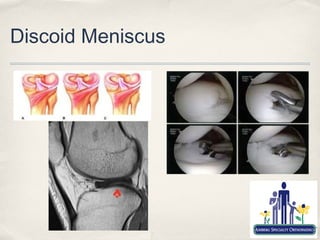
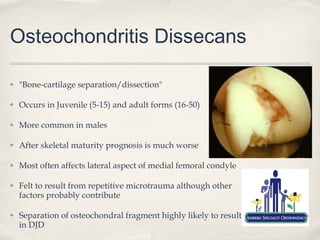
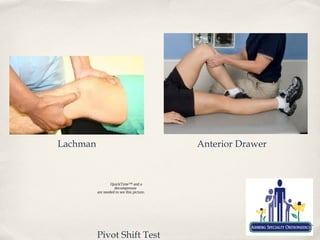
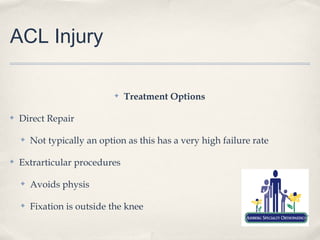
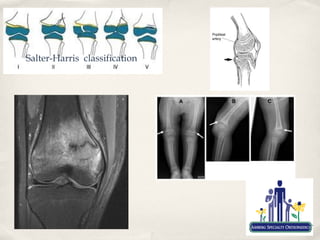
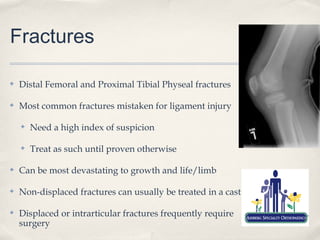
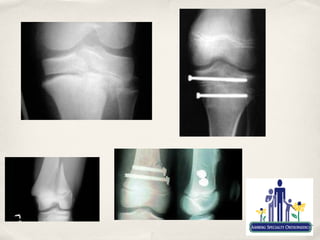
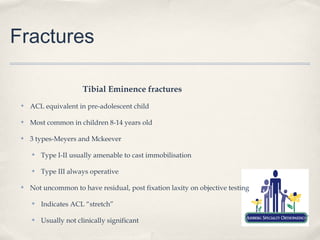
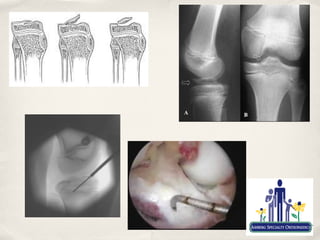
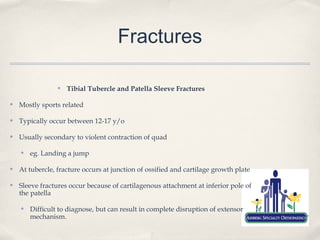
The document discusses common knee problems in paediatric and adolescent patients, emphasizing the importance of understanding growth and development in evaluation and treatment. It covers a spectrum of conditions including acute trauma, overuse syndromes, and specific injuries such as ACL tears, patellar instability, and meniscus issues, alongside treatment options. Key points highlight the differences in injury patterns between genders and the need for careful assessment and management to prevent long-term consequences.