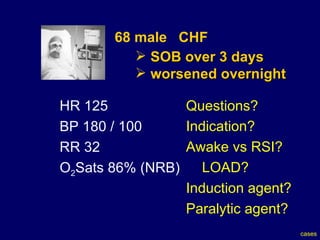
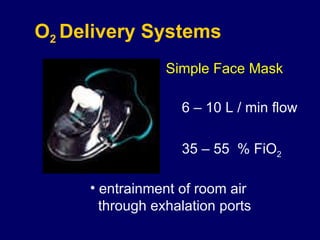
The document appears to be notes from an airway management seminar that discusses various topics related to intubation including indications for intubation, preparation for difficult airways and intubation, choices around rapid sequence intubation versus awake intubation, induction agents, and paralysis agents. Case studies are presented and questions are provided about how to manage each case.