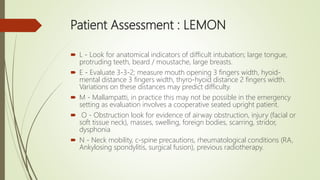
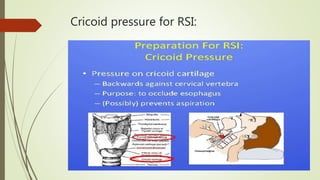
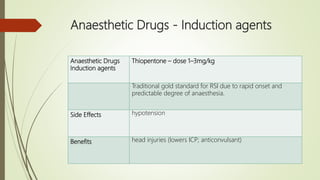
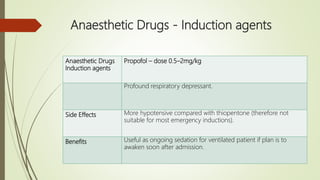
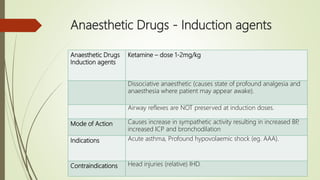
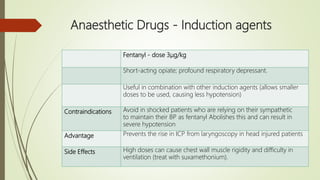
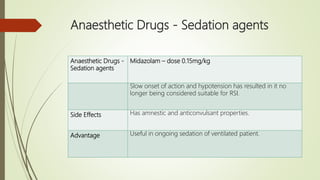
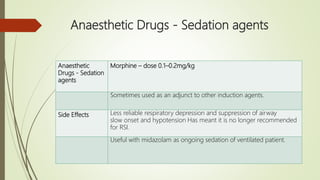
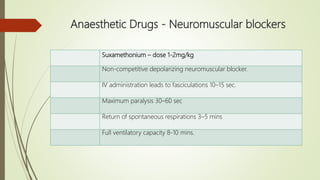
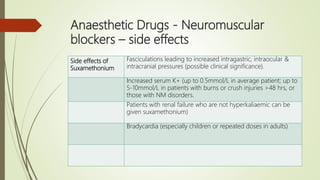
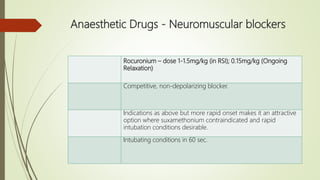
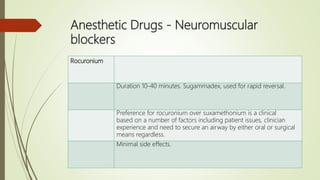
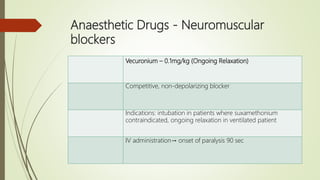
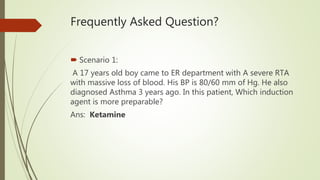
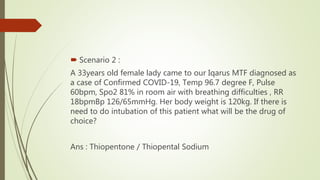
Rapid Sequence Intubation (RSI) aims to secure a definitive airway quickly to minimize risks associated with airway management. The process involves careful patient assessment, preparation, and the use of specific induction agents and neuromuscular blockers, with a clear focus on mitigating challenges during emergency situations. It encompasses team roles for effective execution and successful intubation confirmation through techniques like ETCO2 monitoring.