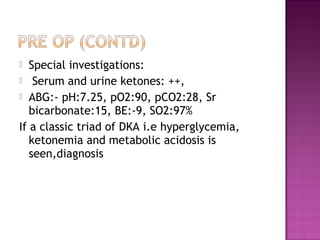
A 55-year-old male presented with pain and swelling in his left foot and lower leg along with abdominal pain and drowsiness. Examination revealed tachycardia, hypotension, tachypnea, and abdominal tenderness. Laboratory findings were consistent with diabetic ketoacidosis (DKA): hyperglycemia, ketonemia, and metabolic acidosis. The patient was diagnosed with DKA likely precipitated by infection and treated with insulin, intravenous fluids, potassium supplementation, and monitoring of electrolytes and glucose levels.