Rapid sequence intubation (RSI) is a process for safely intubating conscious patients by first using sedatives and paralytics. It involves:
1) Preparation with monitoring and drugs ready, preoxygenation to increase oxygen stores before intubation, and pretreatment with lidocaine or fentanyl.
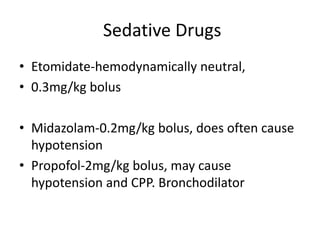
2) Rapidly administering sedatives like etomidate or propofol followed immediately by paralytics like succinylcholine to paralyze before intubation.
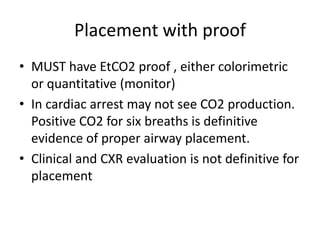
3) Properly positioning the patient, intubating, and confirming placement with end-tidal CO2 monitoring before securing the tube and providing post-intubation management.