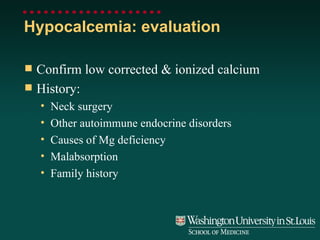
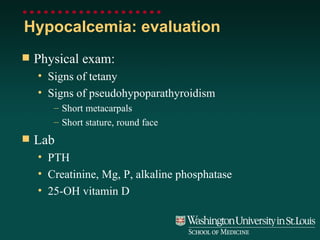
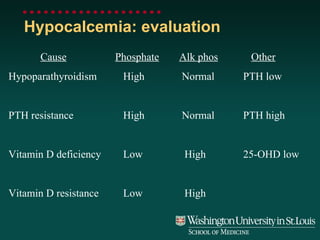
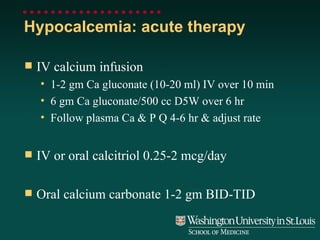
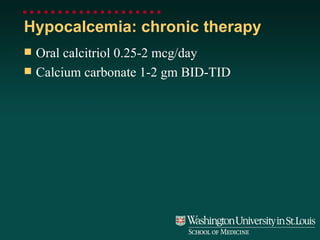
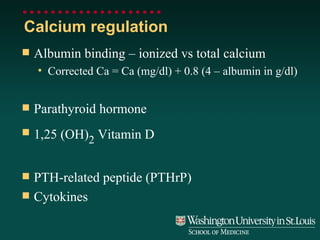
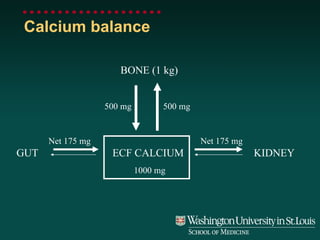
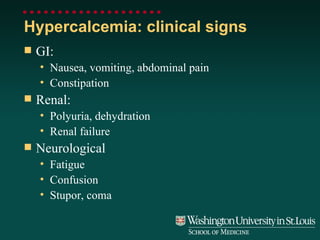
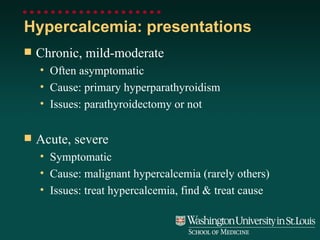
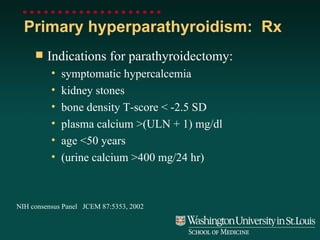
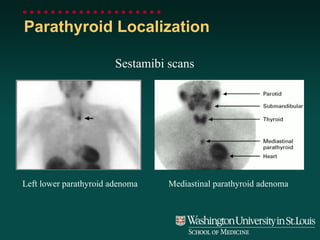
Calcium levels in the body are tightly regulated through the actions of parathyroid hormone (PTH), vitamin D, and other factors. Disorders can cause either hypercalcemia (high calcium levels) or hypocalcemia (low calcium levels). Primary hyperparathyroidism, where the parathyroid glands overproduce PTH, is a common cause of hypercalcemia and may require parathyroid surgery. Malignancy is another major cause through the action of PTH-related peptide. Severe hypercalcemia requires rehydration and drugs to reduce bone resorption and calcium levels. Hypocalcemia can result from hypoparathyroidism or resistance to PTH/vitamin D
![Severe hypercalcemia: Principles of therapy Expand ECF volume Increase urinary calcium excretion Decrease bone resorption Indications for therapy Symptoms of hypercalcemia Plasma [Ca] >12 mg/dl](https://image.slidesharecdn.com/clutter-1233835478704700-3/85/Calcium-disorder-18-320.jpg)
![Severe hypercalcemia: therapy Restore ECF volume Normal saline rapidly Positive fluid balance >2 liters in first 24 hr Saline diuresis Normal saline 100-200 ml/hr (replace potassium) Zoledronic acid 4 mg IV over 15 min if plasma [Ca] >14 mg/dl or >12 mg/dl after rehydration Monitor plasma calcium QD Myeloma or vitamin D toxicity: prednisone 30 mg BID](https://image.slidesharecdn.com/clutter-1233835478704700-3/85/Calcium-disorder-19-320.jpg)