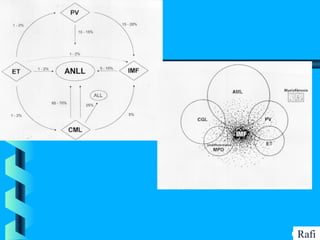
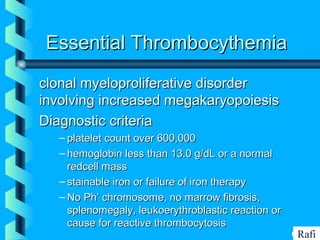
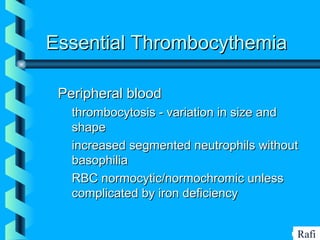
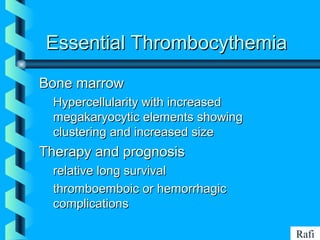
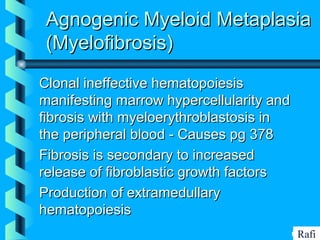
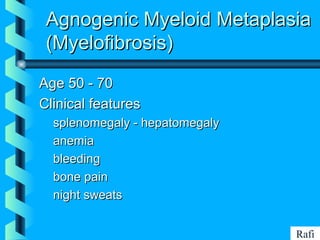
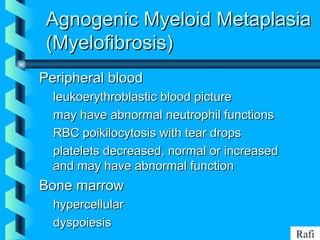
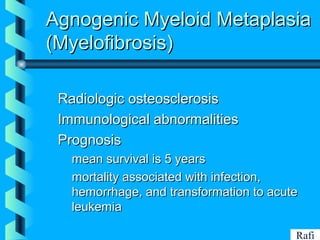
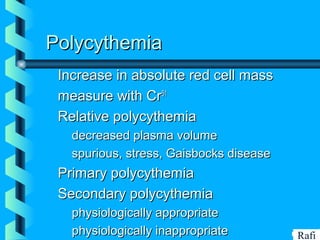
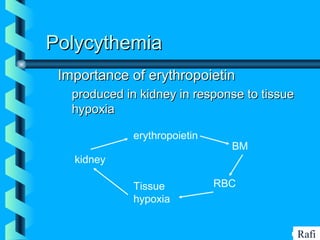
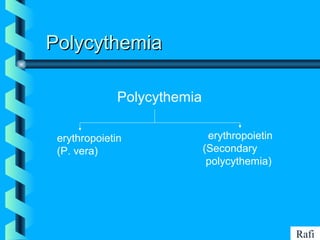
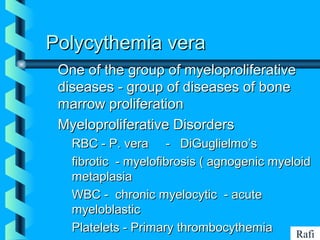
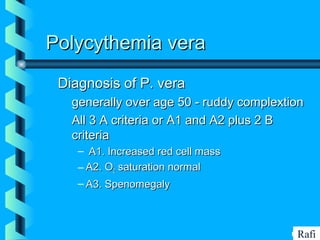
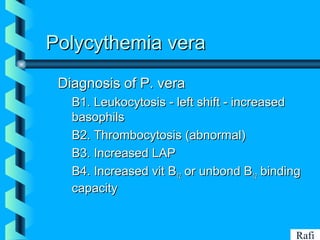
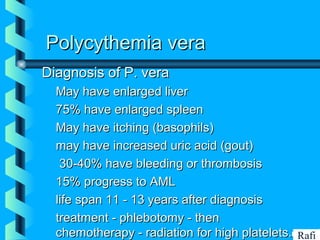
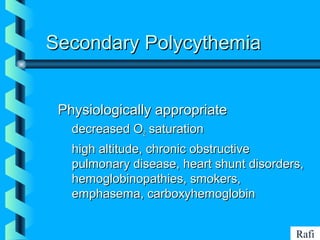
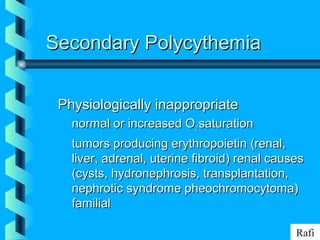
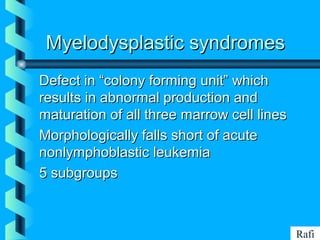
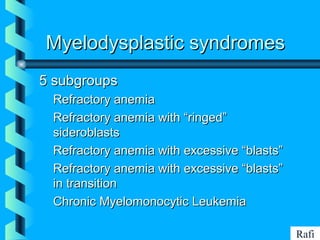
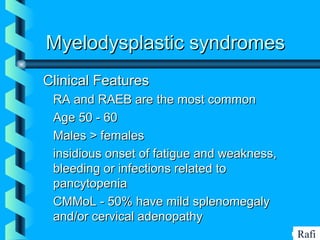
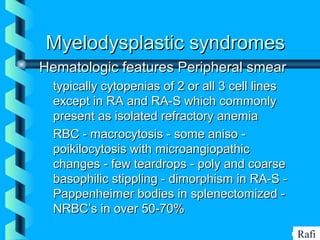
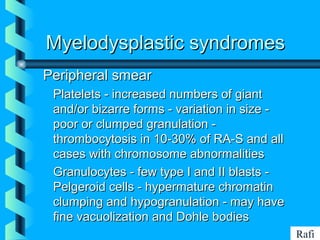
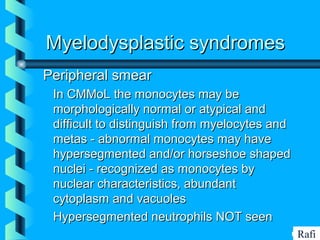
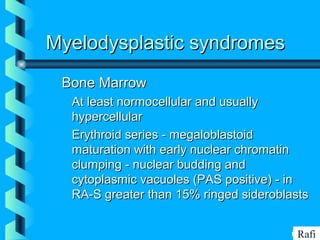
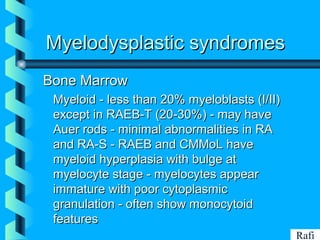
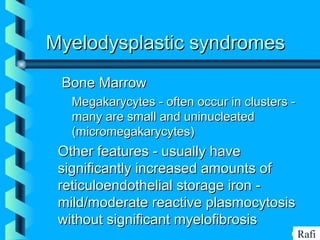
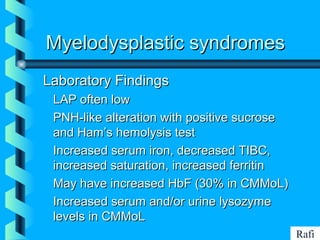
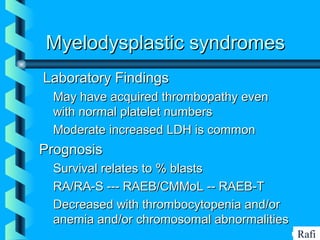
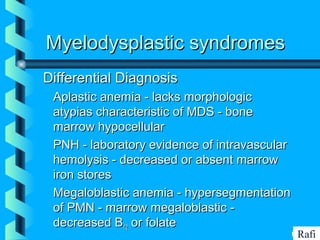
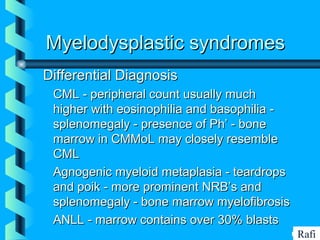
This document discusses several types of myeloproliferative disorders and myelodysplastic syndromes. It provides details on the diagnosis and features of essential thrombocythemia, polycythemia vera, myelofibrosis, myelodysplastic syndromes, and secondary polycythemia. Key information covered includes diagnostic criteria, peripheral blood and bone marrow findings, clinical manifestations, and prognosis for each condition.