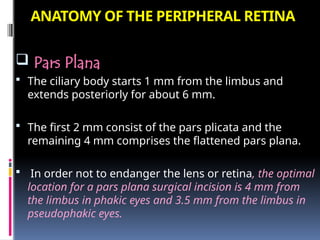
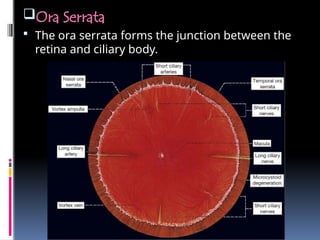
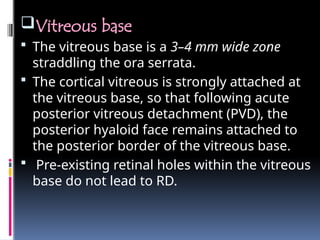
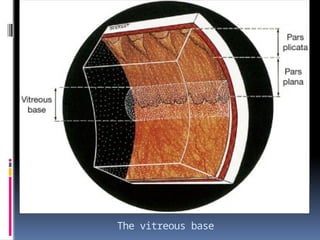
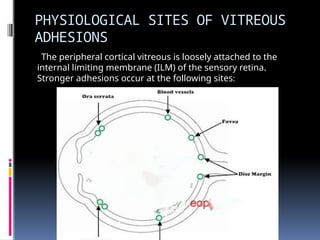
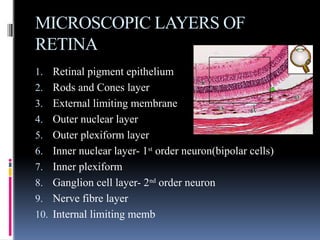
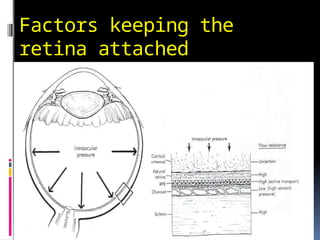
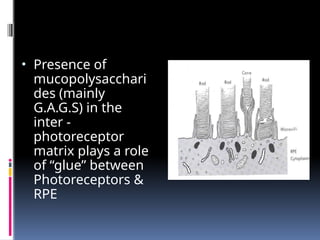
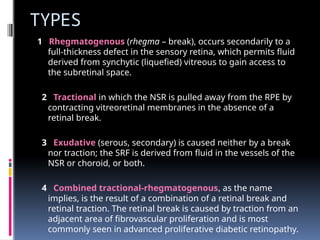
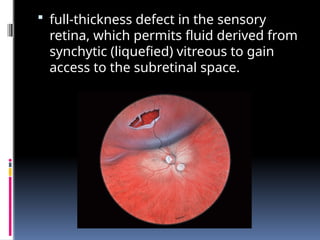
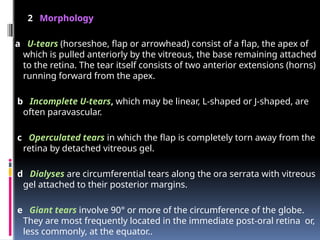
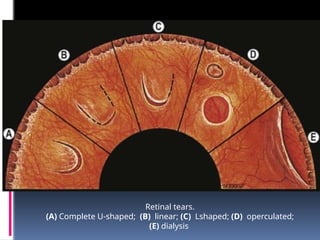
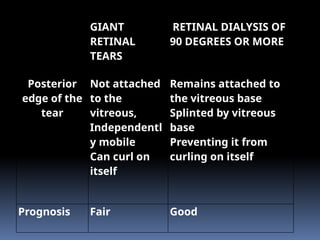
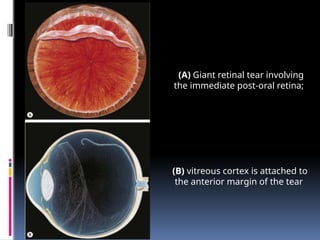
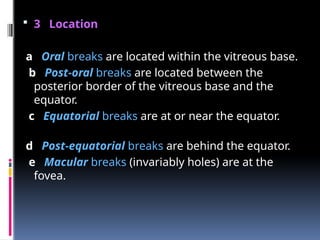
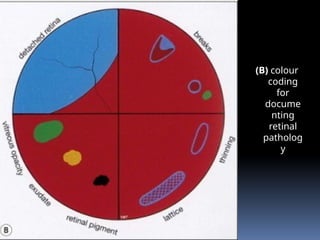
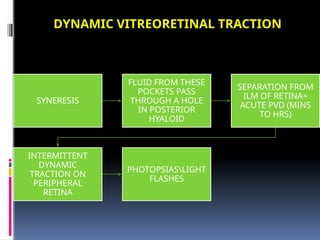
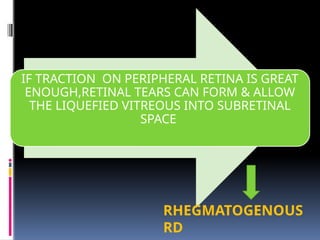
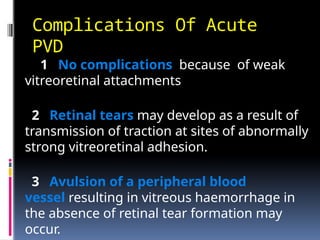
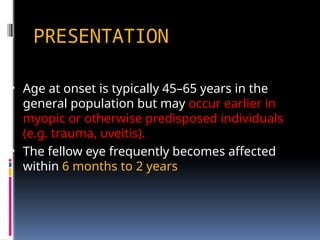
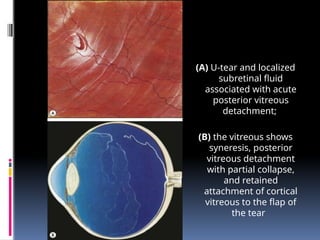
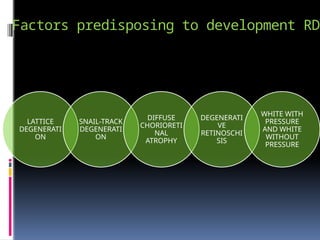
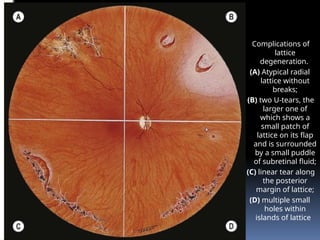
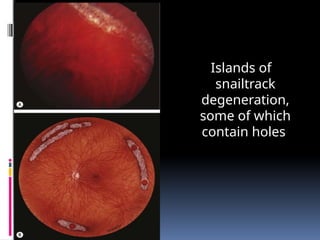
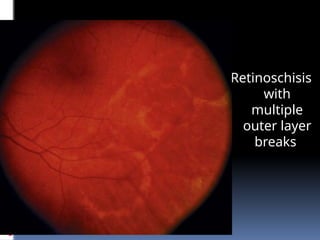
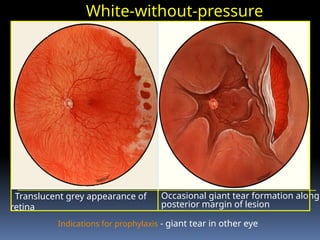
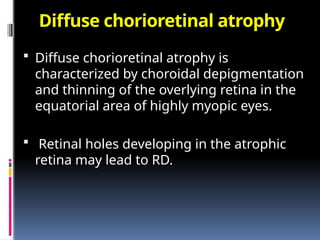
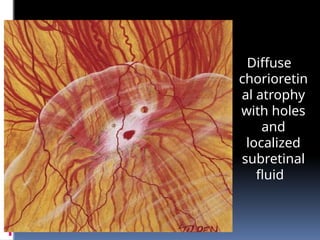
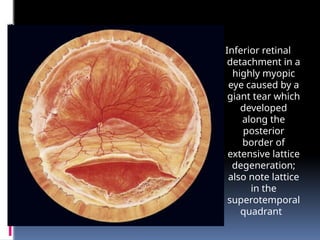
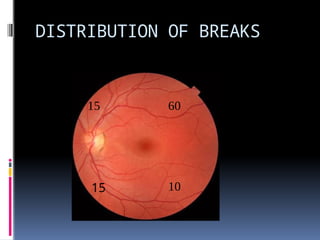
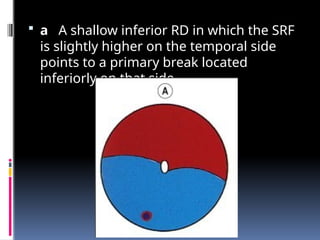
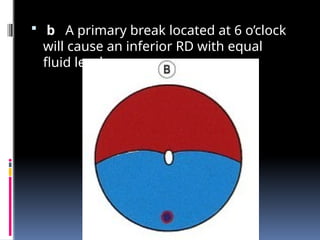
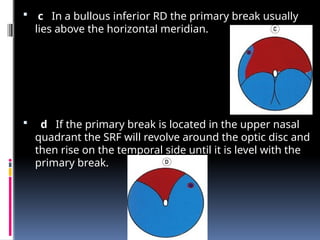
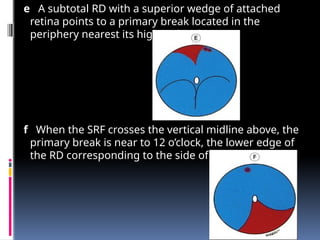
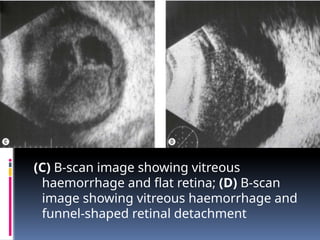
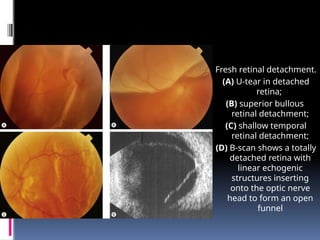
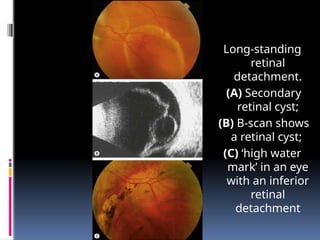
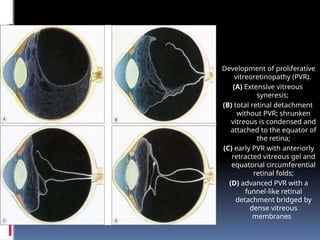
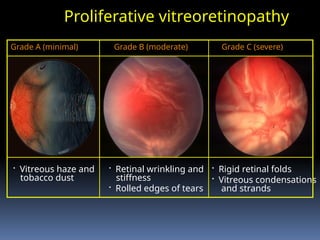
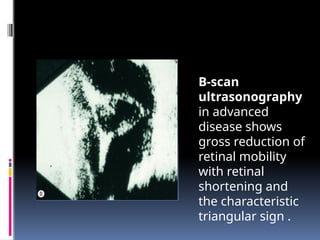
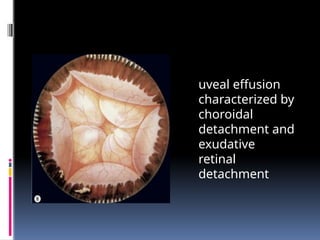
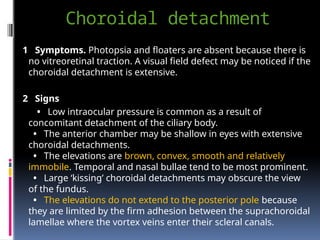
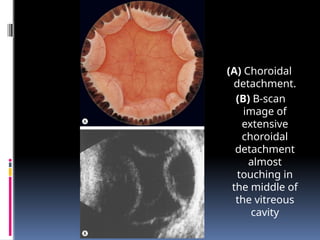
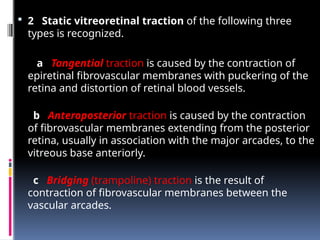
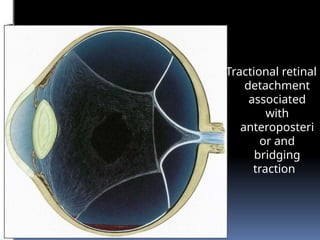
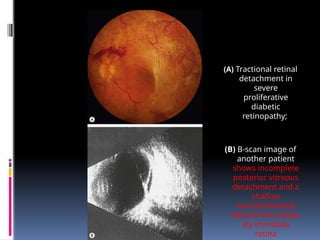
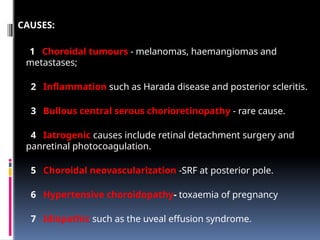
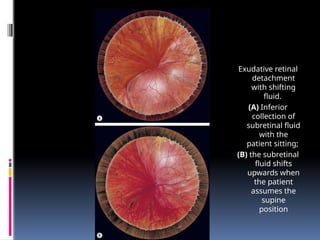
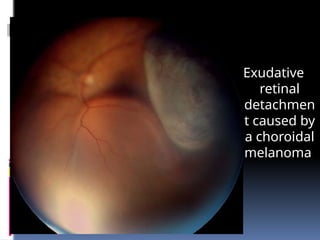
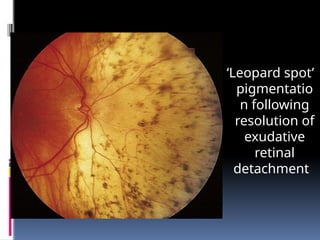
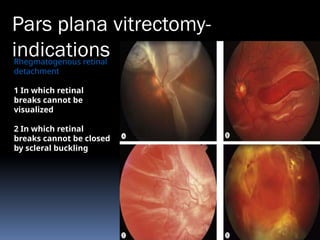
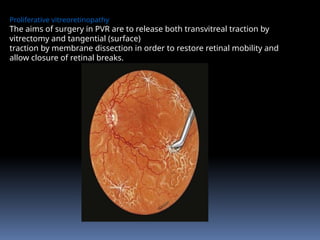
The document comprehensively discusses retinal detachment, detailing its anatomy, types (rhegmatogenous, tractional, and exudative), mechanisms, and clinical evaluation through ultrasonography. It outlines the causes, implications of posterior vitreous detachments, and the pathophysiology of various retinal breaks, including factors leading to retinal detachment and the characteristics of related complications. Additionally, it covers management considerations and the significance of predisposing conditions, particularly in myopic eyes.