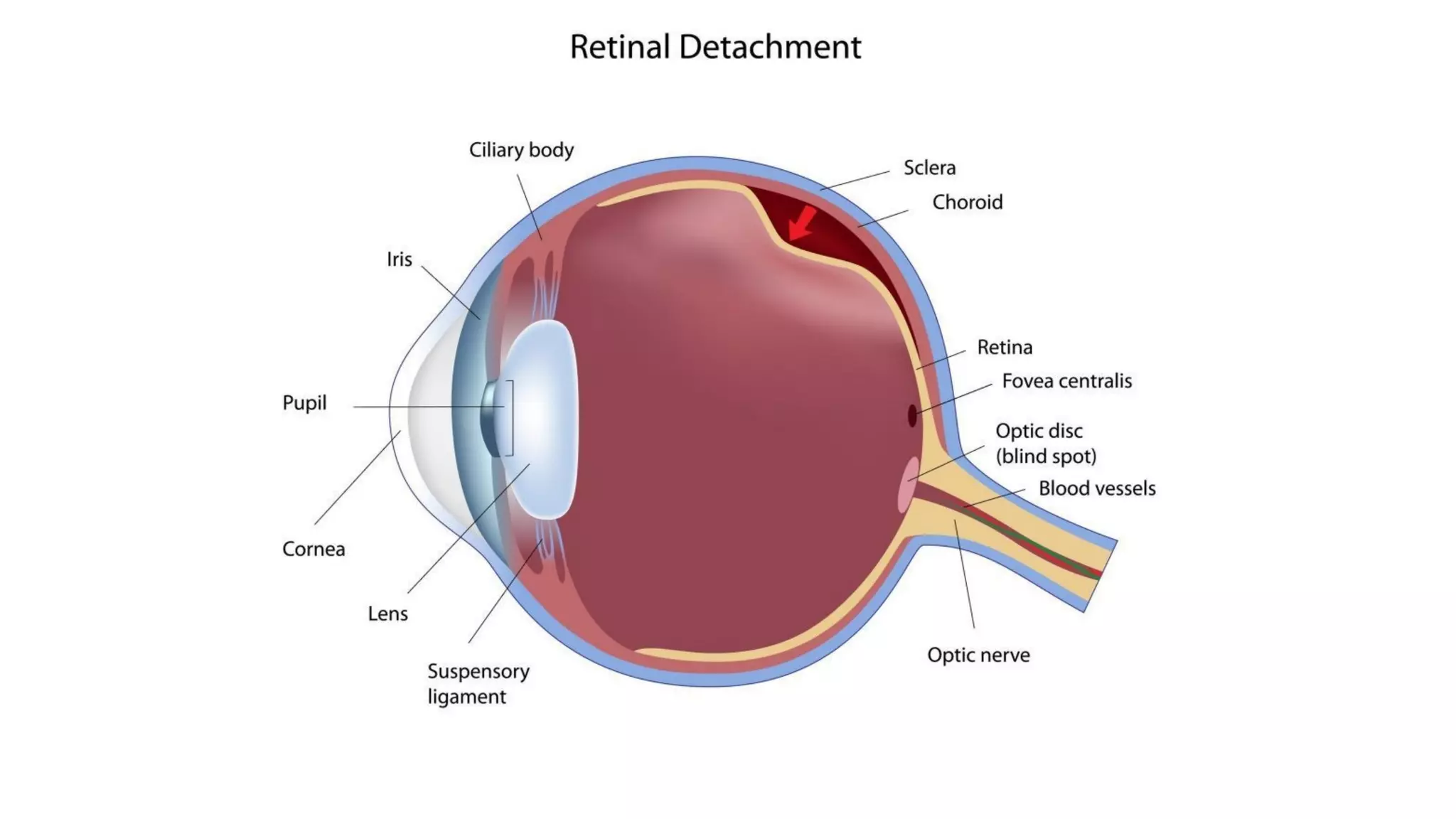
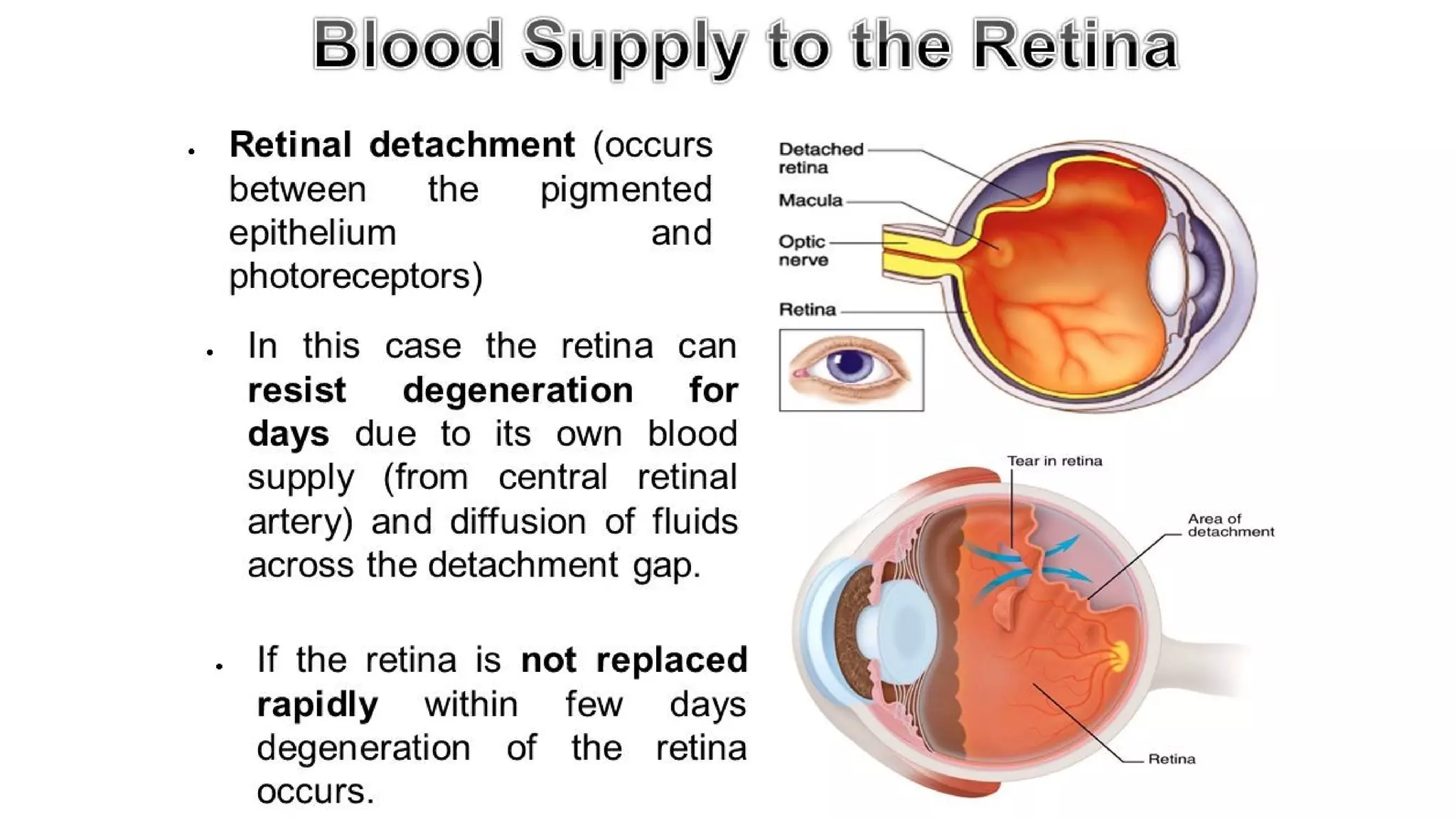
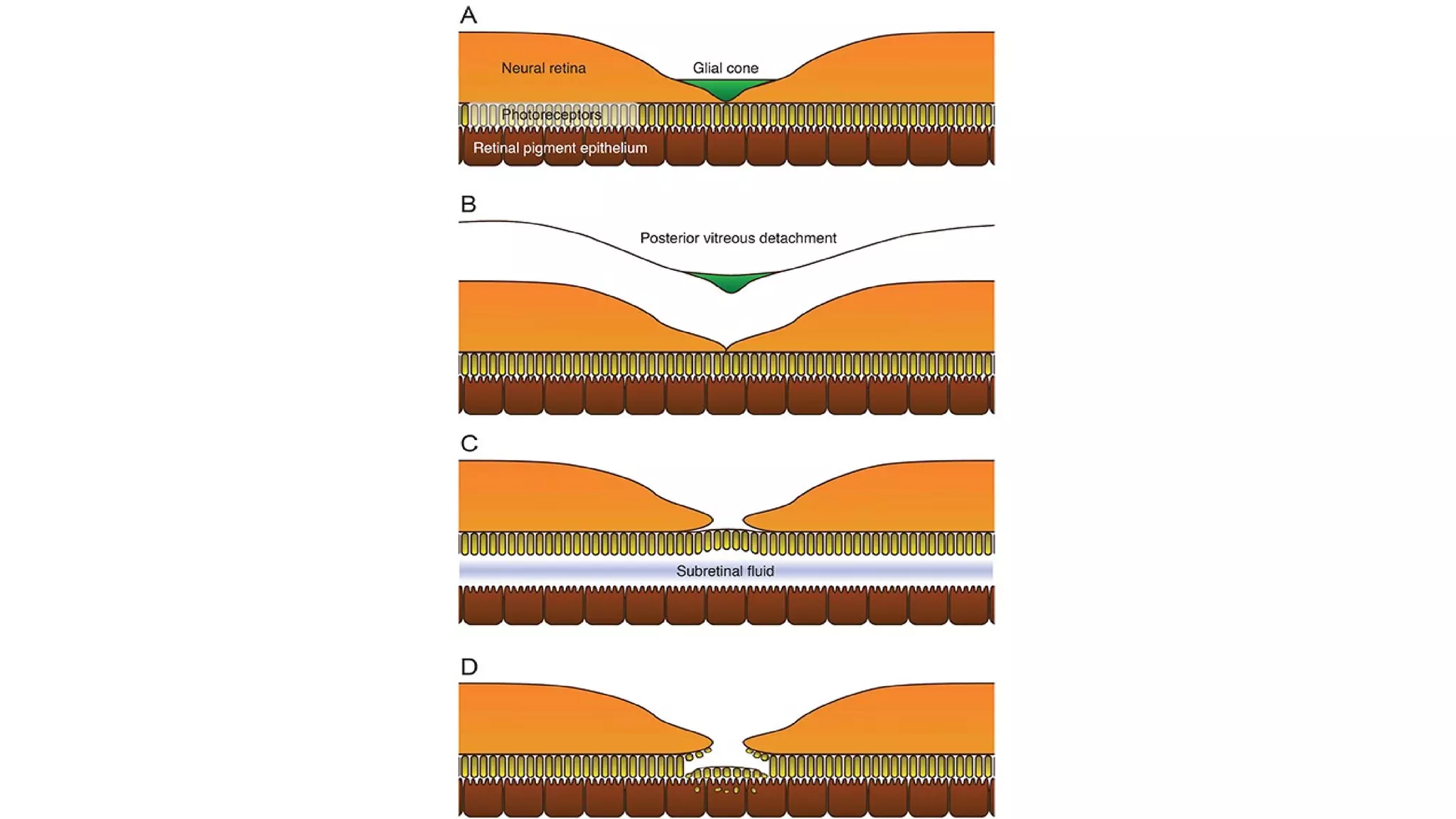
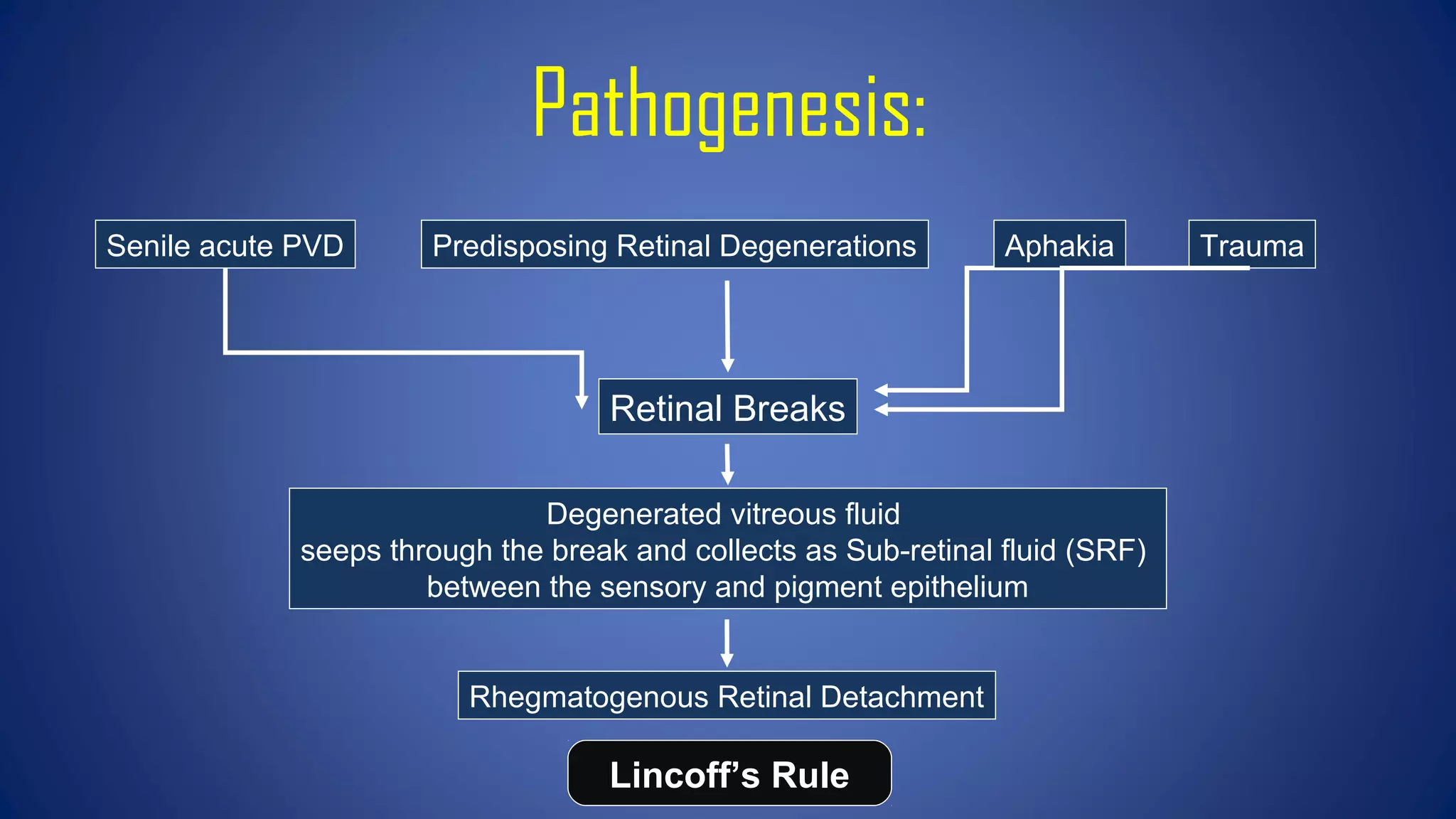
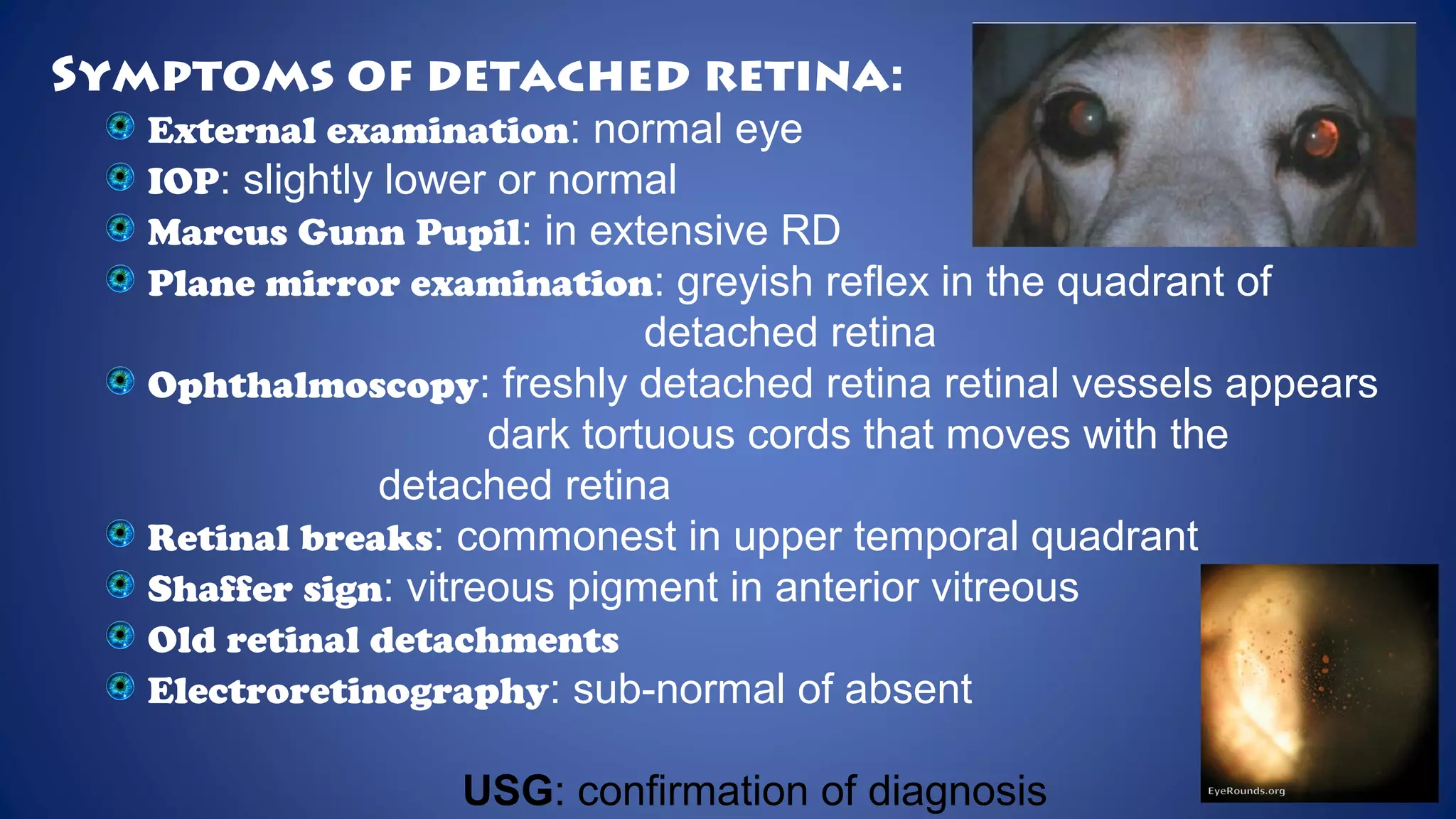
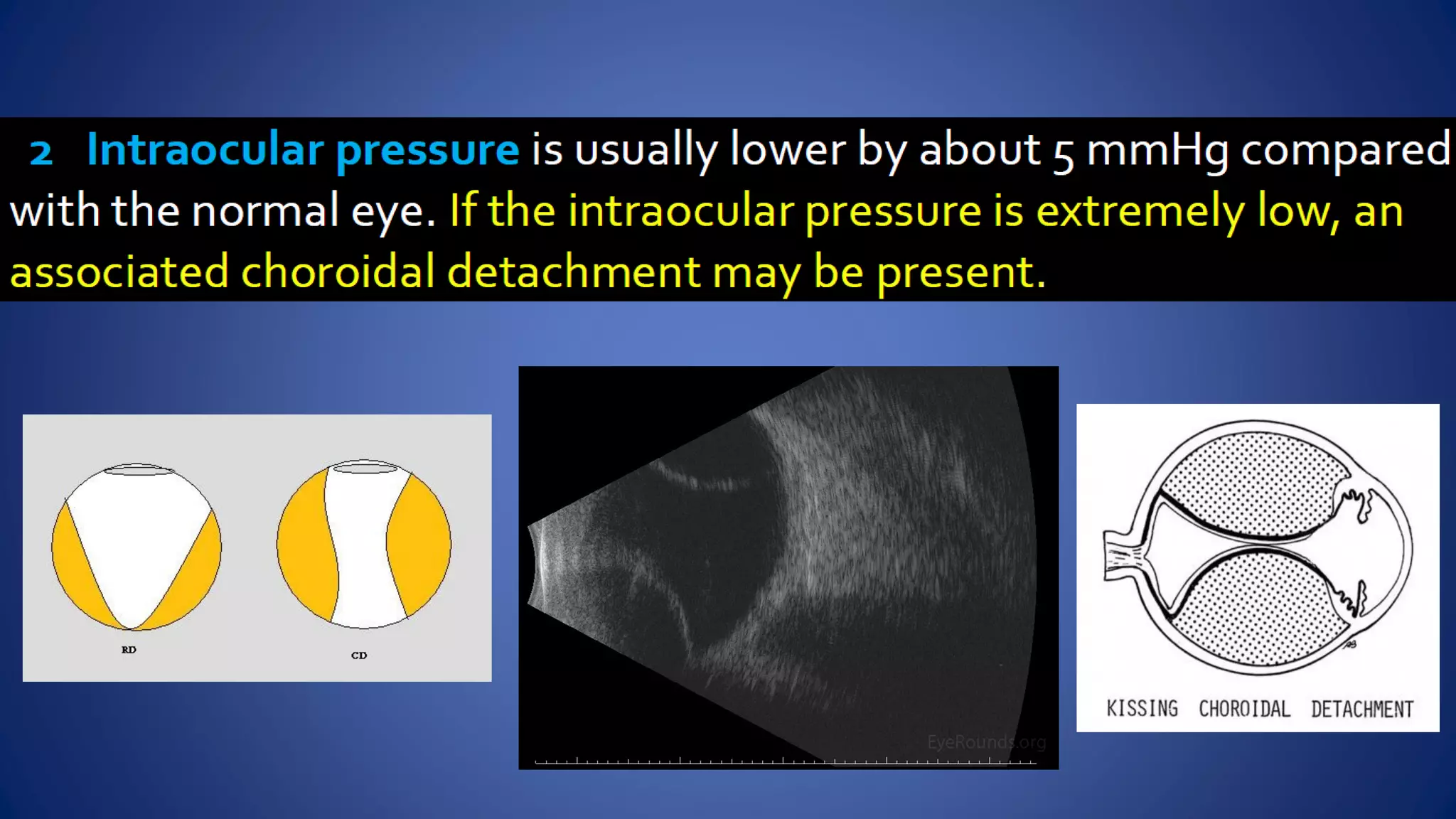
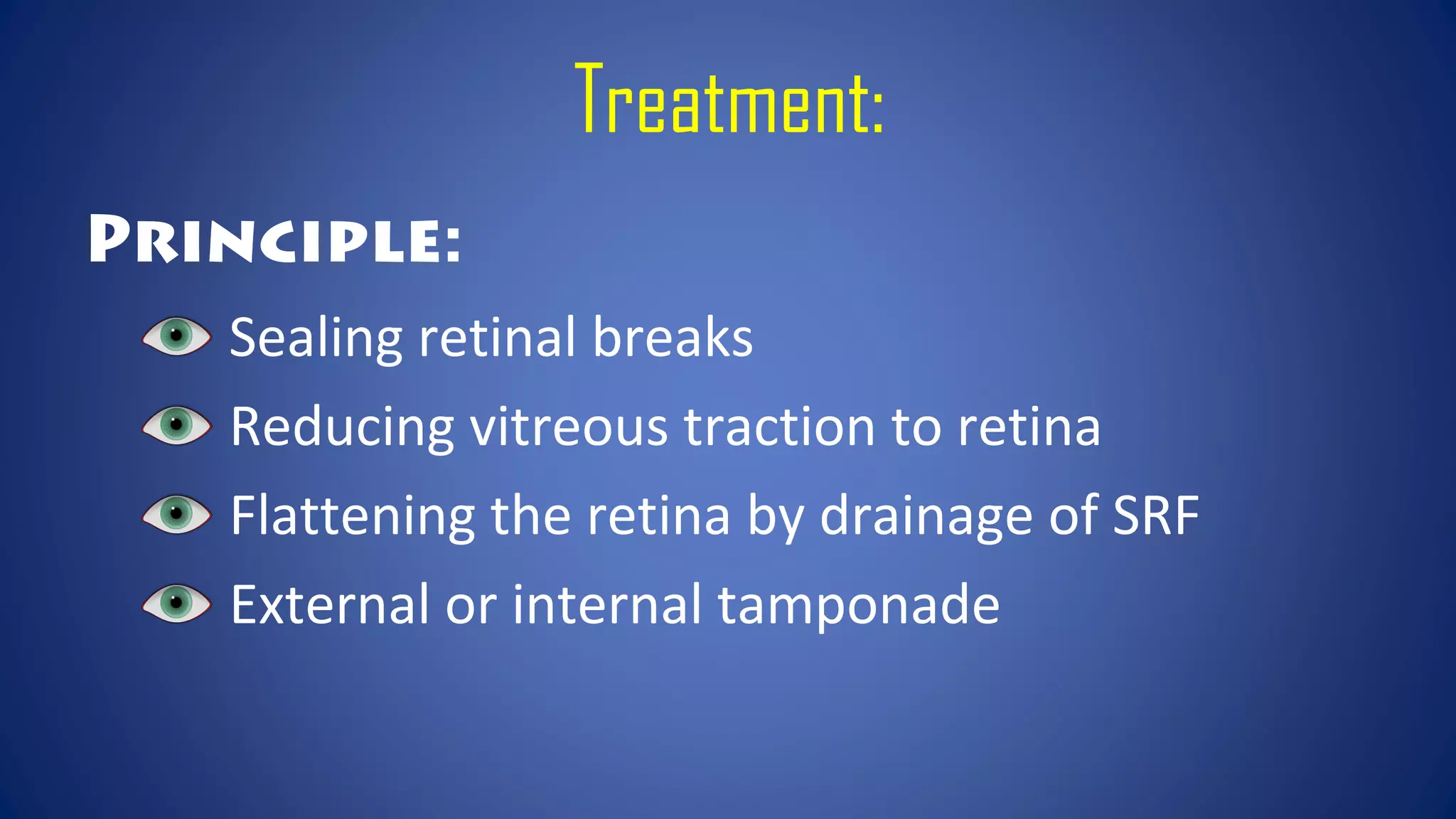
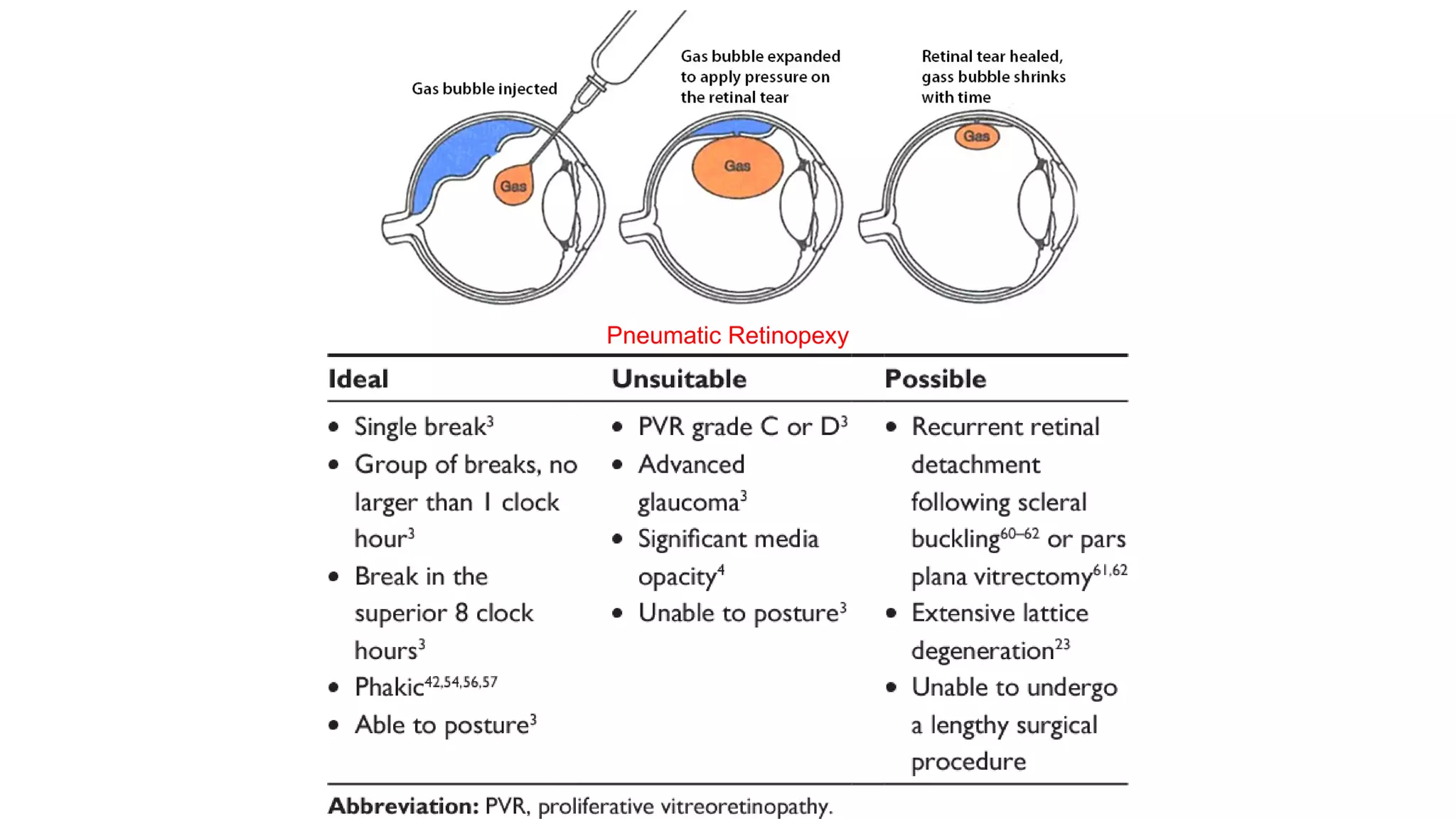
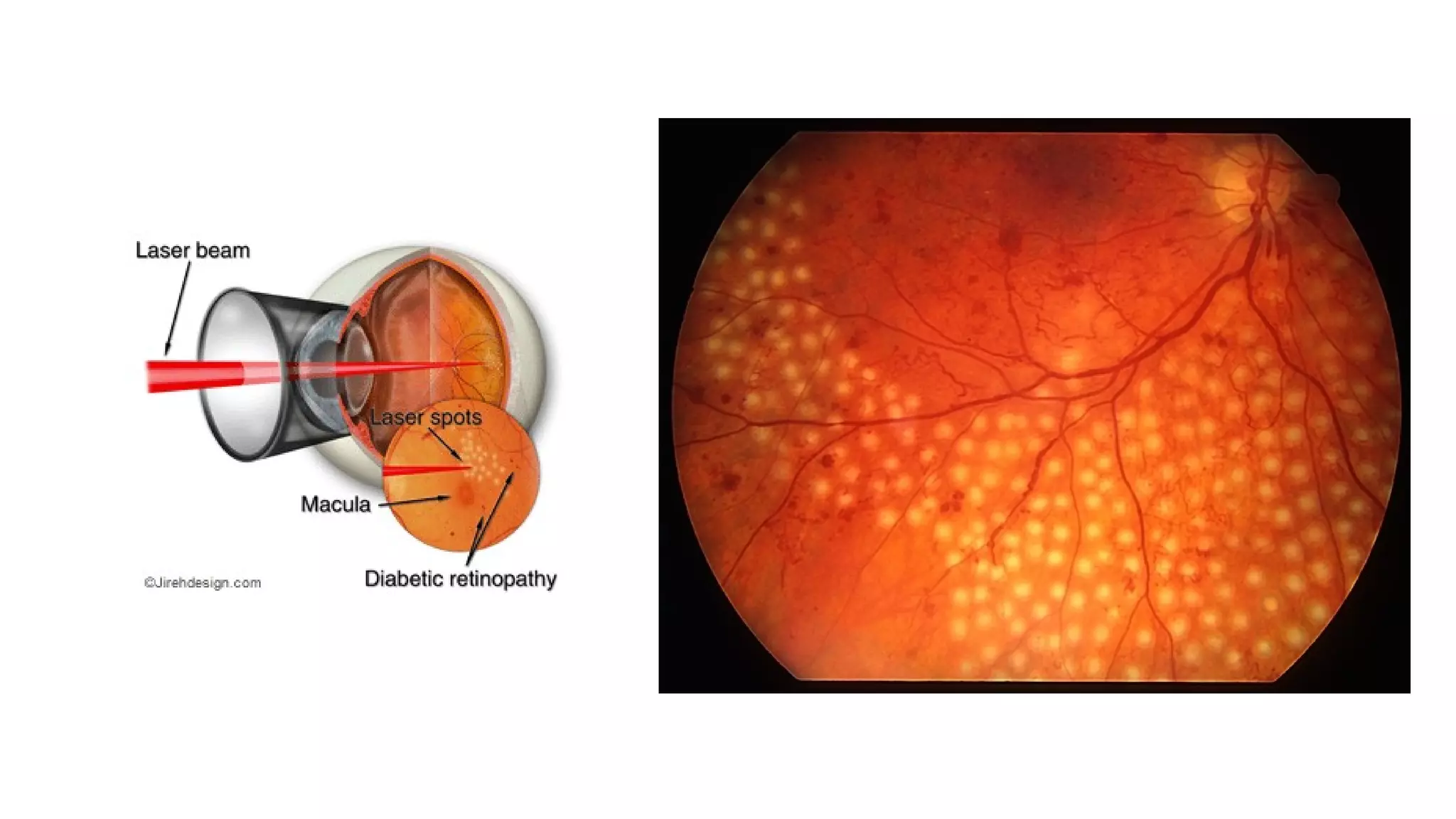
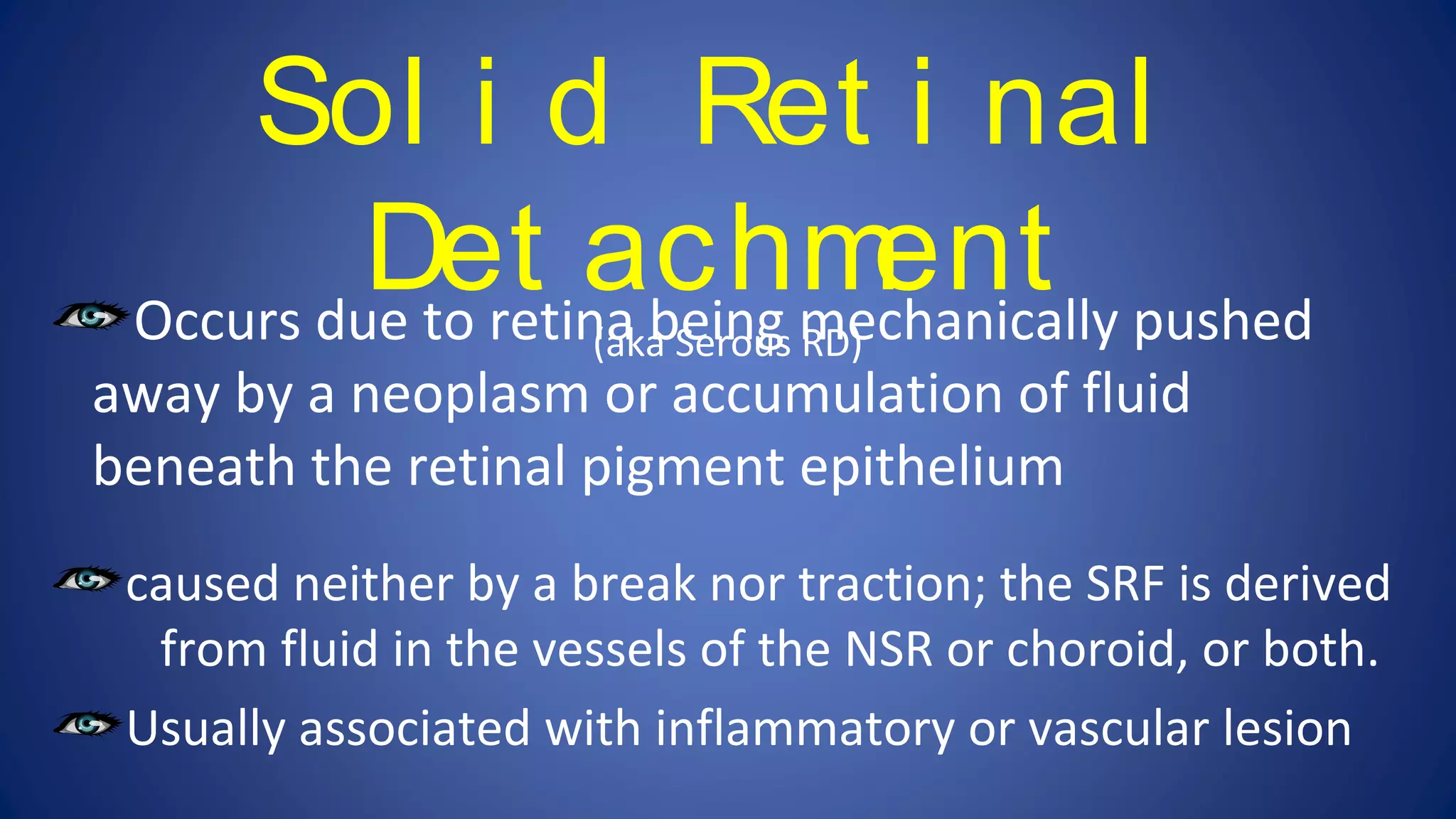
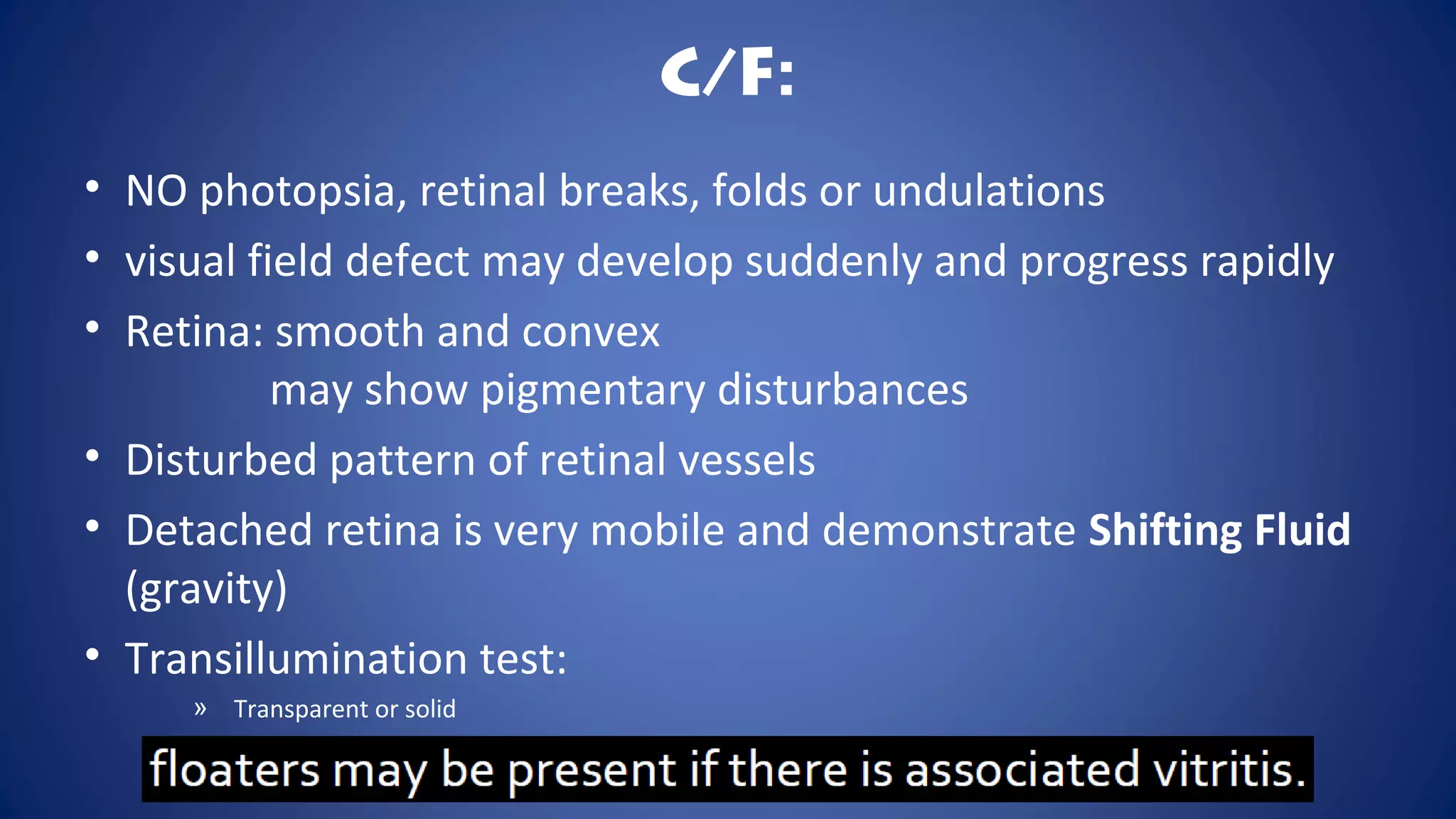
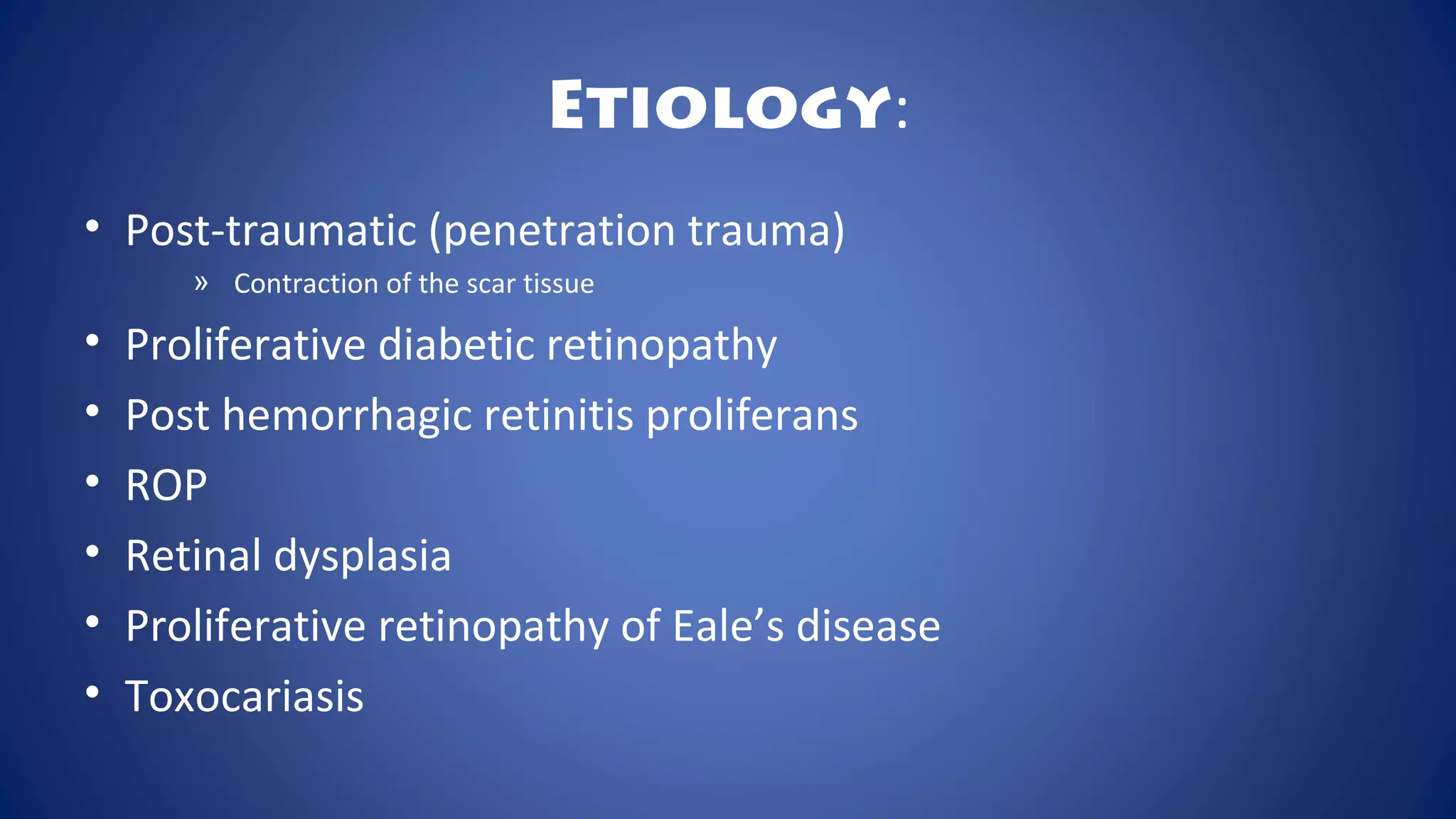
This document discusses different types of retinal detachment. Rhegmatogenous retinal detachment is the most common type and occurs when there is a break or tear in the retina that allows fluid from the vitreous to enter the subretinal space. Tractional retinal detachment occurs when the retina is pulled away from the retinal pigment epithelium due to contraction of fibrous tissue in the vitreous. Exudative retinal detachment occurs when fluid accumulates beneath the retinal pigment epithelium due to inflammation or vascular issues. The document outlines causes, symptoms, examinations, and treatments for each type of retinal detachment.