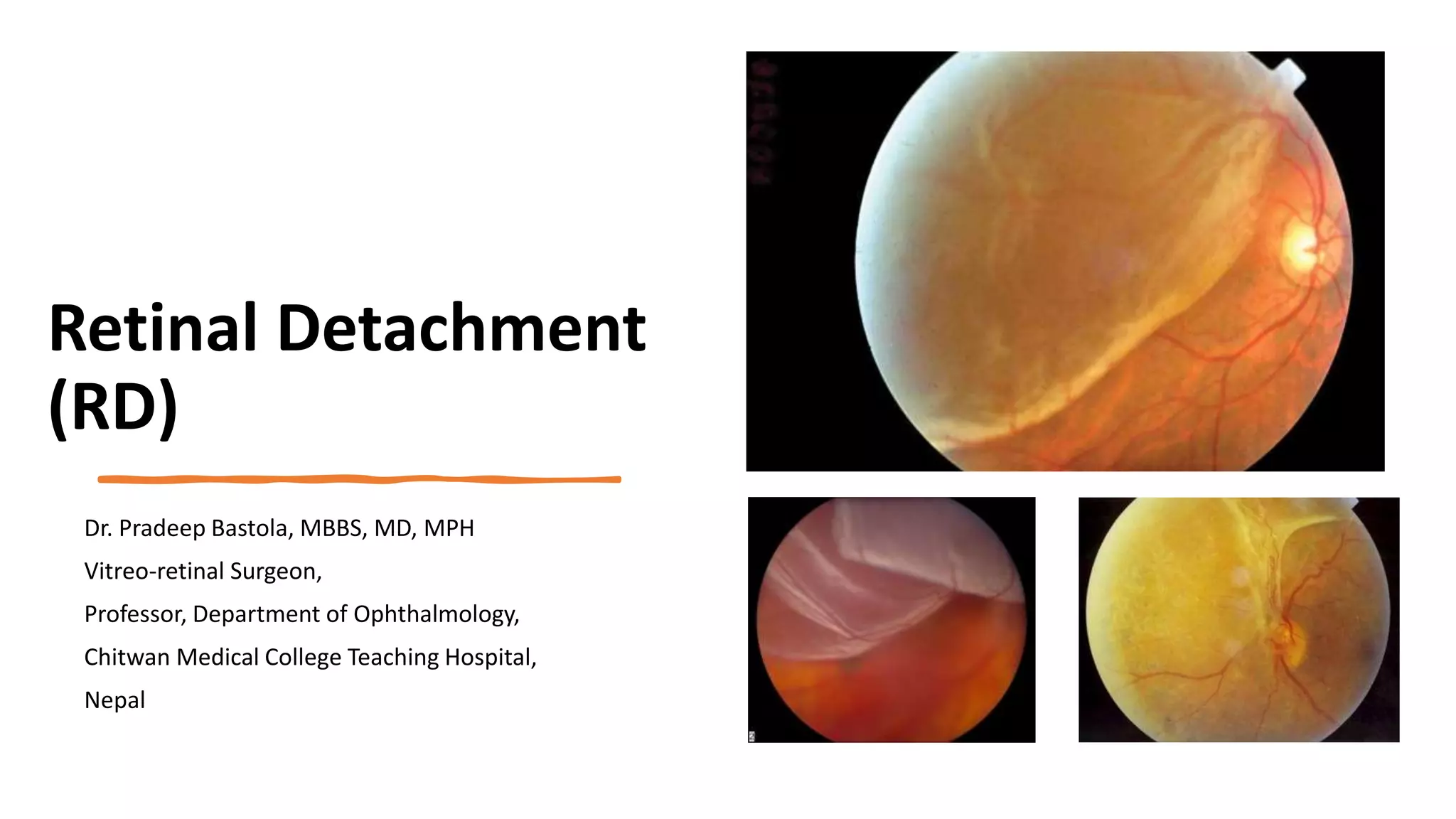
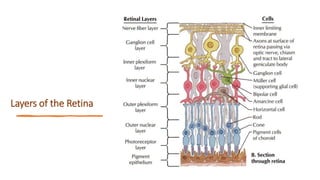
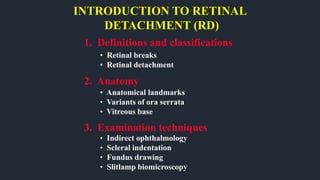
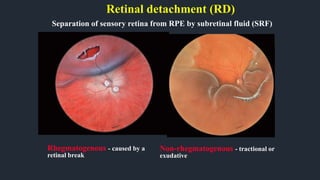
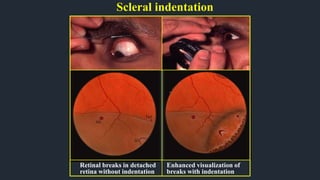
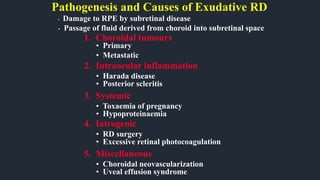
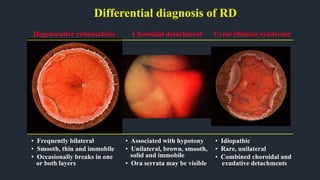
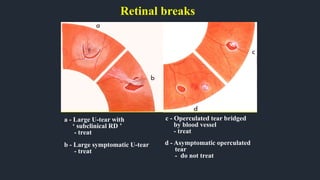
1. Retinal detachment occurs when the neurosensory retina separates from the retinal pigment epithelium, usually due to a retinal break that allows fluid to enter the subretinal space.
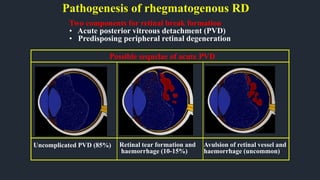
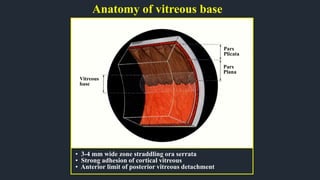
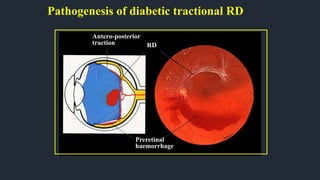
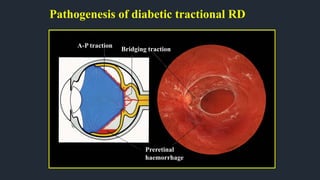
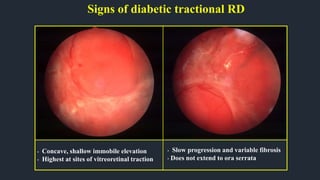
2. Rhegmatogenous retinal detachment is caused by a retinal break or tear, while tractional retinal detachment is caused by vitreoretinal traction without a break.
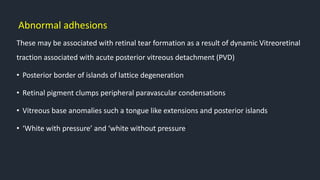
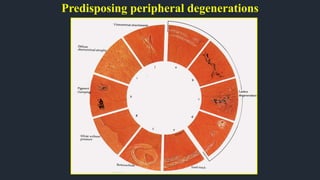
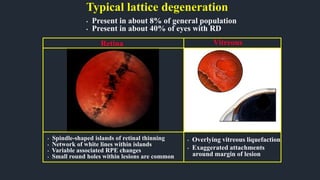
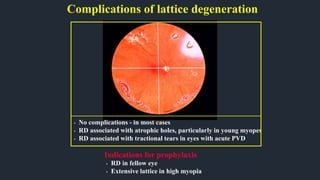
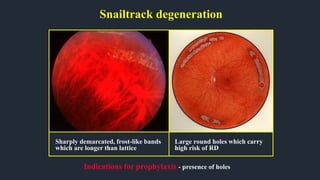
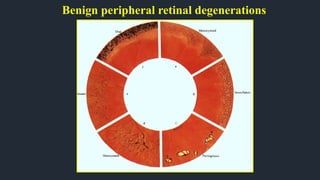
3. Risk factors for retinal detachment include high myopia, posterior vitreous detachment, lattice degeneration, retinal tears or breaks, retinal disease, and prior ocular surgery or trauma.