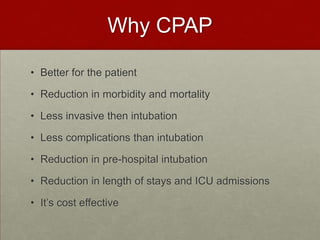
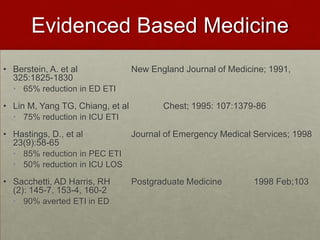
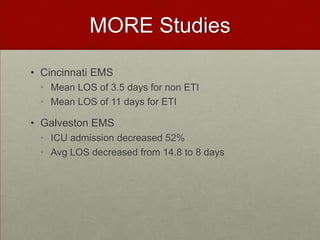
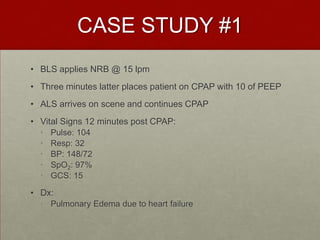
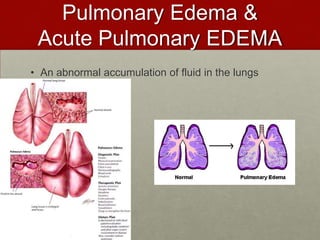
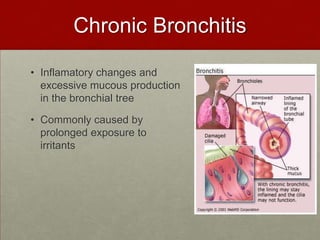
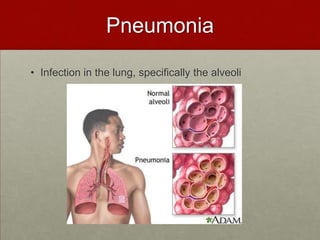
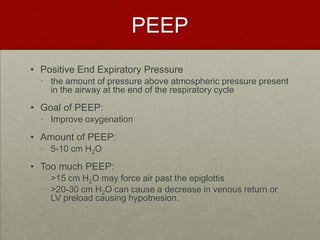
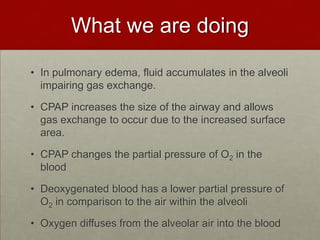
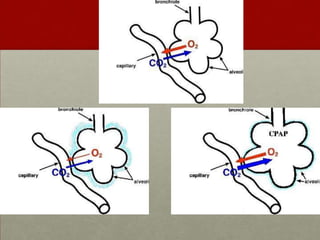
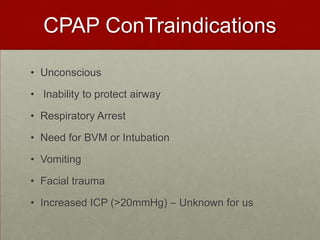
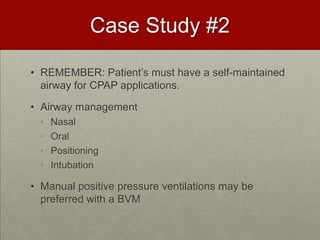
CPAP can help patients with respiratory distress breathe easier by applying continuous positive airway pressure. It works by splinting open the airways and lungs to allow for better gas exchange and oxygenation of the blood. Studies show CPAP can reduce intubation rates, ICU admissions, and hospital lengths of stay for patients with pulmonary edema from heart failure and other respiratory conditions like pneumonia. While CPAP may not resolve the underlying problem, it can significantly improve symptoms and buy time to treat the condition further. Proper application and monitoring of patients on CPAP is important to watch for potential complications.