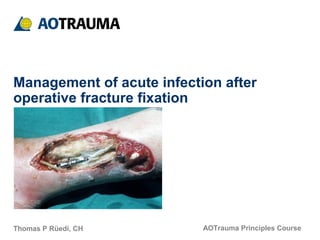
This document discusses principles for managing acute infection after operative fracture fixation. It notes an infection rate of 1-2% for closed fractures and 6-7% for open fractures. Risk factors for surgical site infection include older age, comorbidities, drugs, prior infections, and emergency operations. Factors contributing to acute infection include contamination, a medium for bacteria to grow, mechanical instability, and dead soft tissues. Strict protocols around cleaning, masking, handwashing, and isolating MRSA patients can reduce contamination risk. Careful surgical technique, debridement, hemostasis, and temporary fixation can address other risk factors. Signs of acute infection include swelling, pain, fever and elevated inflammatory markers. Aggressive wound revision