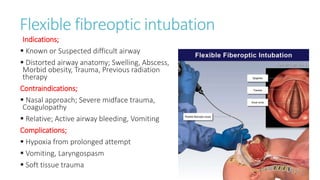
This document discusses tracheal intubation and rapid sequence intubation (RSI). RSI involves rapidly sedating and paralyzing a patient to facilitate endotracheal intubation. The key steps of RSI are preoxygenation, induction with sedatives, paralysis with neuromuscular blocking agents, protection of the airway with cricoid pressure during intubation, confirmation of proper endotracheal tube placement, and post-intubation management and securing of the airway. RSI aims to minimize risks of aspiration and facilitate safe and rapid intubation in emergency situations.