This document provides information on airway management techniques. It discusses:
- The importance of airway management and oxygenation in resuscitation.
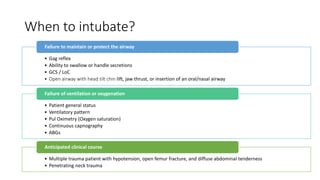
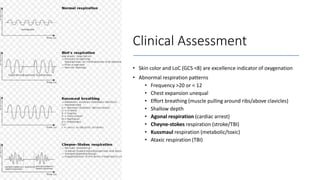
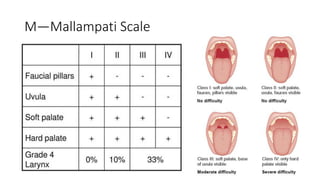
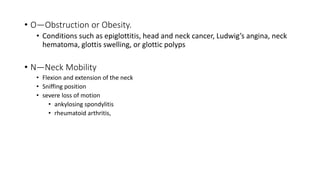
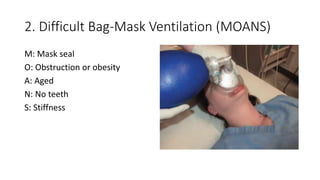
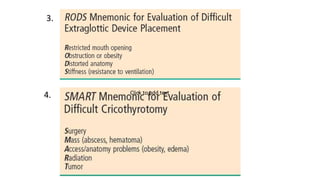
- Clinical assessments for determining when to intubate a patient.
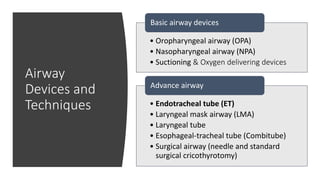
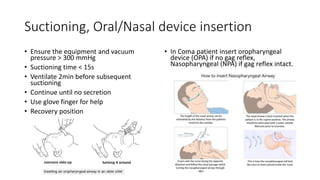
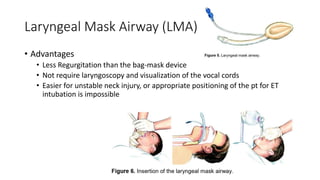
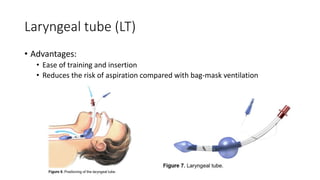
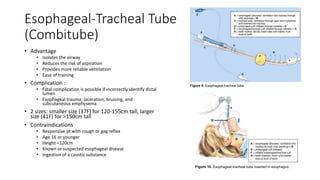
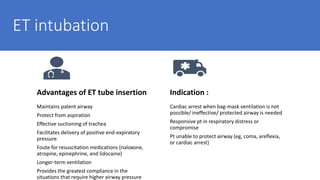
- Basic and advanced airway devices like oropharyngeal airways, endotracheal tubes, and laryngeal mask airways.
- Techniques for opening the airway like head tilt/chin lift and jaw thrust maneuvers.
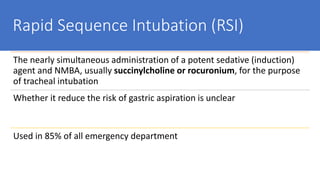
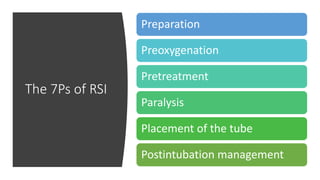
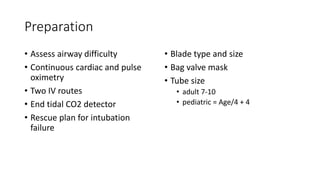
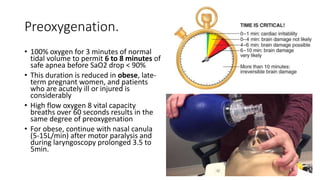
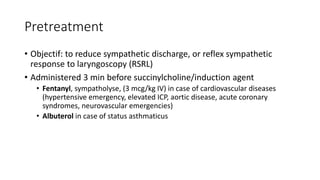
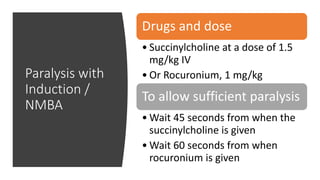
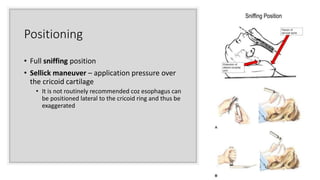
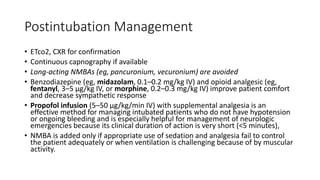
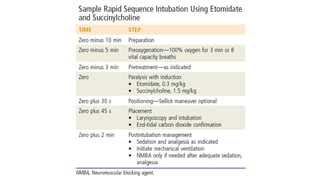
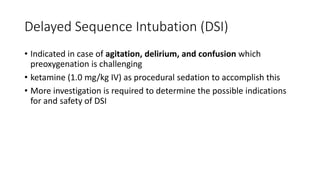
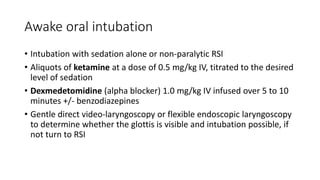
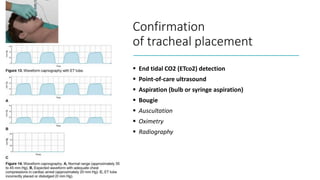
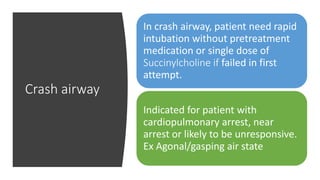
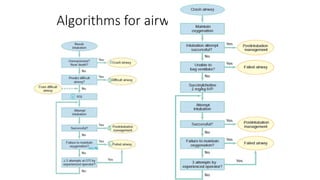
- Methods for intubation including rapid sequence intubation and its components.
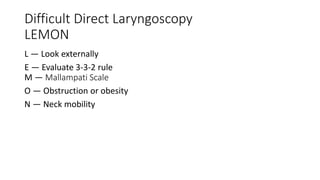
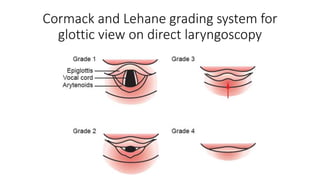
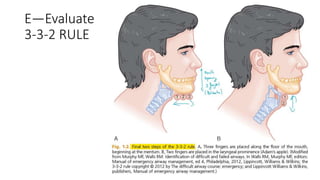
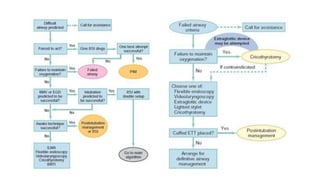
- Approaches for difficult airways including video laryngoscopy and rescue techniques if intubation fails.