This document describes the procedure for radical cystectomy. It provides details on:
- The indications for radical cystectomy including muscle-invasive bladder cancer and refractory non-muscle invasive disease.
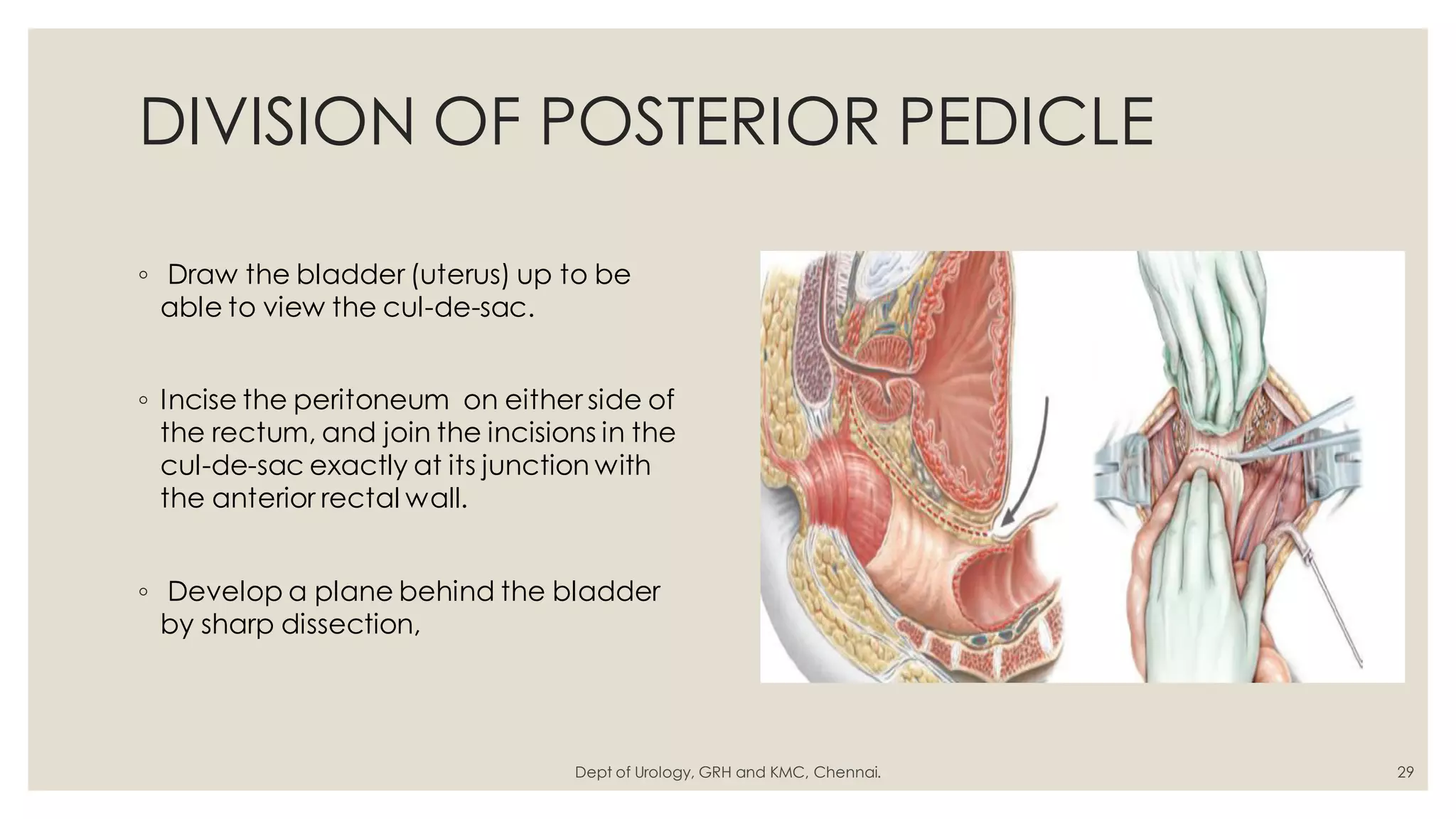
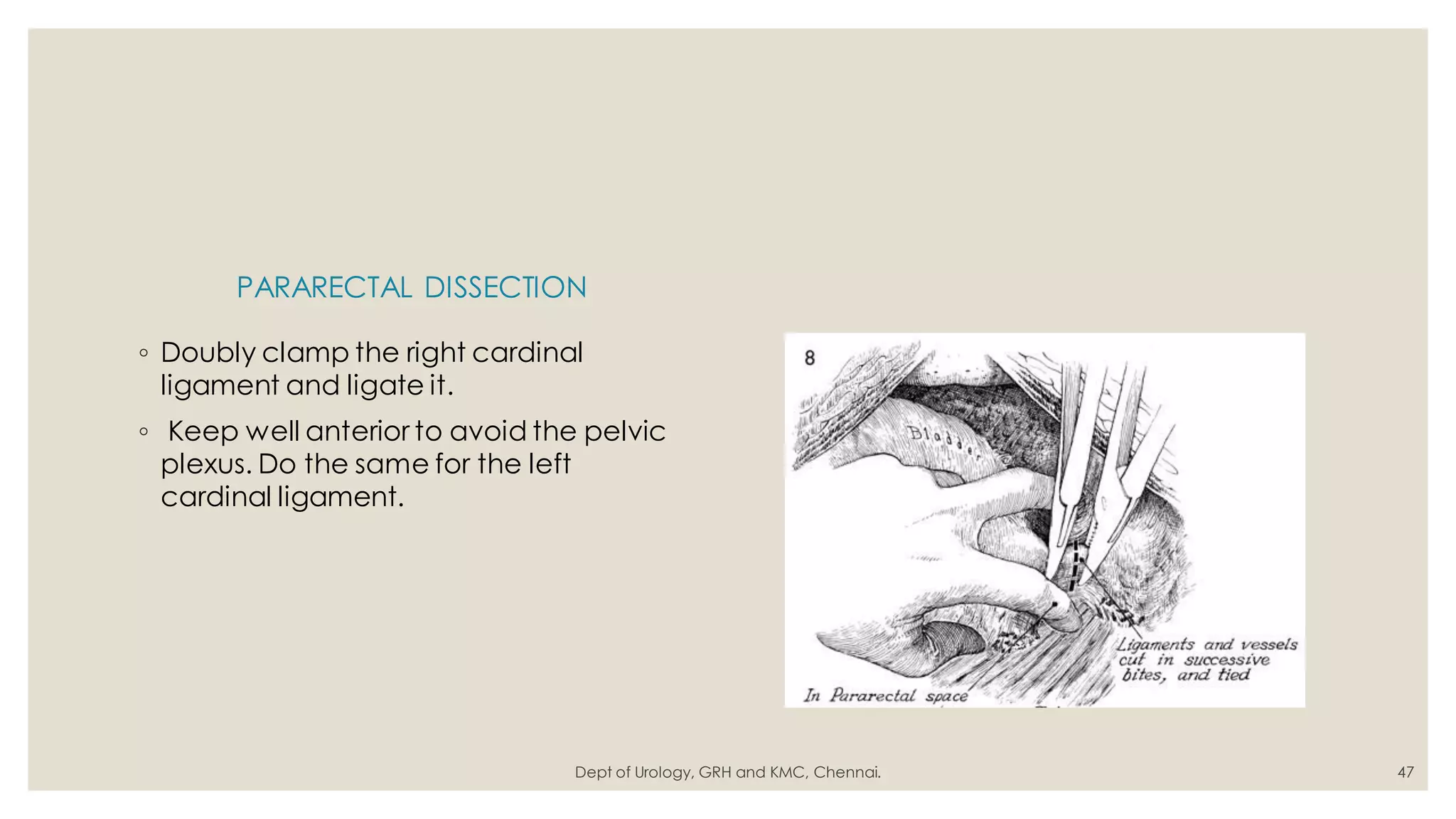
- The surgical technique for radical cystectomy in males, including lymph node dissection, division of the bladder pedicles, and removal of the bladder and prostate.
- The surgical technique for radical cystectomy in females, including ligation of the round ligaments, division of the ureters, and removal of the bladder, uterus, and vaginal cuff.
- Key steps like mobilization of the bowel, identification and preservation of the ureters, and closure are discussed.