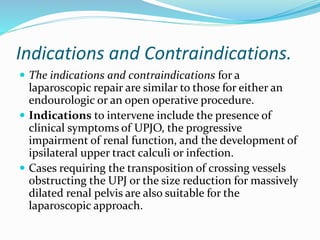
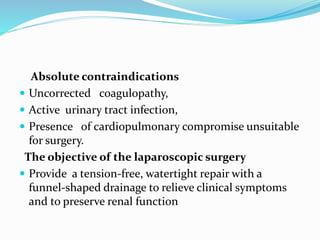
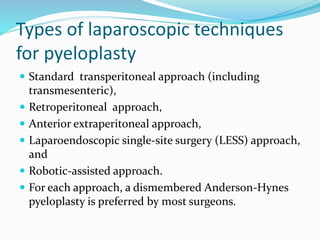
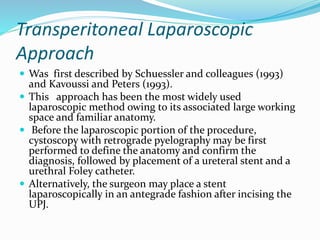
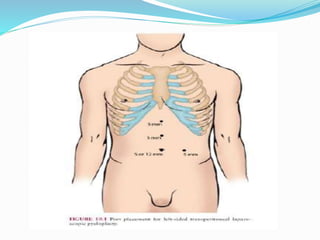
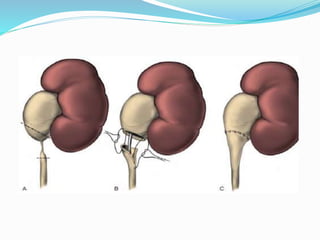
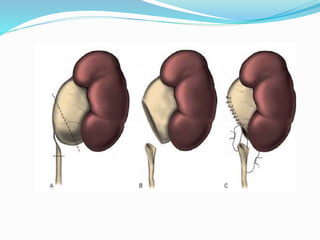
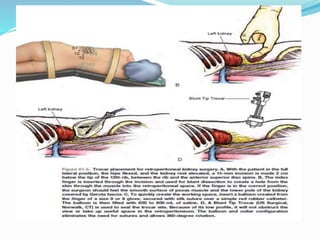
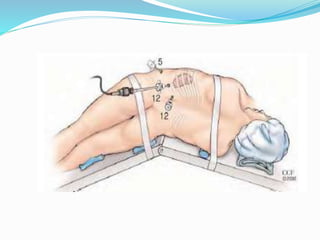
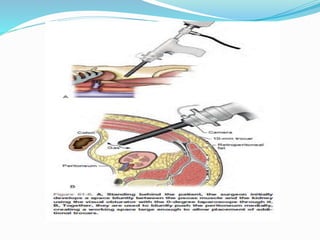
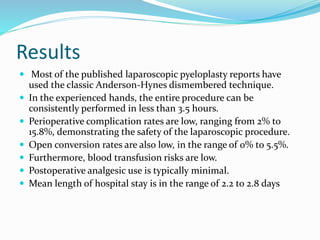
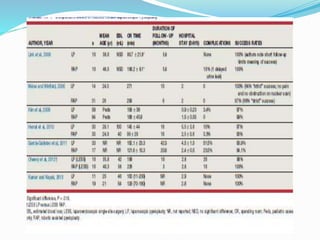
This document discusses urinary tract obstruction, specifically ureteropelvic junction obstruction (UPJO). It covers the causes, evaluation, and surgical treatment options for UPJO, with a focus on laparoscopic pyeloplasty. Key points include that UPJO can be congenital or acquired, and indications for intervention include symptoms, impaired renal function, stones or infection. Laparoscopic pyeloplasty is a less invasive alternative to open surgery that provides comparable success rates while reducing morbidity. The procedure involves mobilizing the colon, dissecting the ureter, and performing a dismembered pyeloplasty reconstruction.