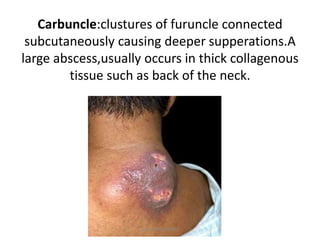
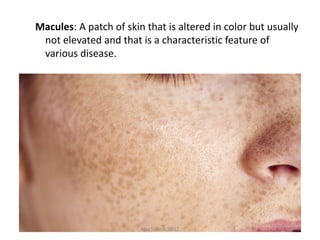
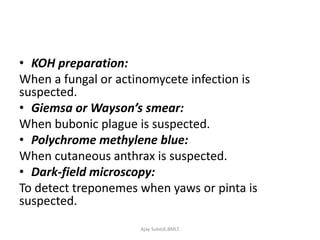
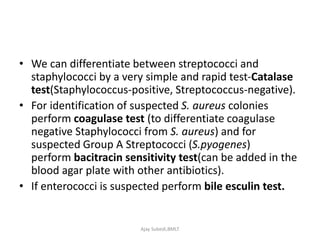
The document provides a detailed overview of pyogenic infections, characterized by severe inflammation and pus formation due to bacterial causes. It discusses various types of infections, common pathogens, and the body's inflammatory response, highlighting specific infections like folliculitis, impetigo, and abscesses. Additionally, it covers laboratory diagnosis, specimen collection methods, and transport/storage protocols for effective microbial analysis.