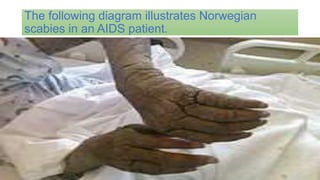
This document discusses various skin infections, including parasitic, bacterial, and fungal infections. It focuses on scabies, impetigo, and cellulitis. Scabies is caused by mites burrowing under the skin and can be transmitted through direct contact. Symptoms include intense itching and rashes. Impetigo is a bacterial infection common in children that causes sores or blisters. Cellulitis is a bacterial skin infection that causes swelling and redness, often on the lower legs. Both impetigo and cellulitis are usually treated with oral antibiotics.