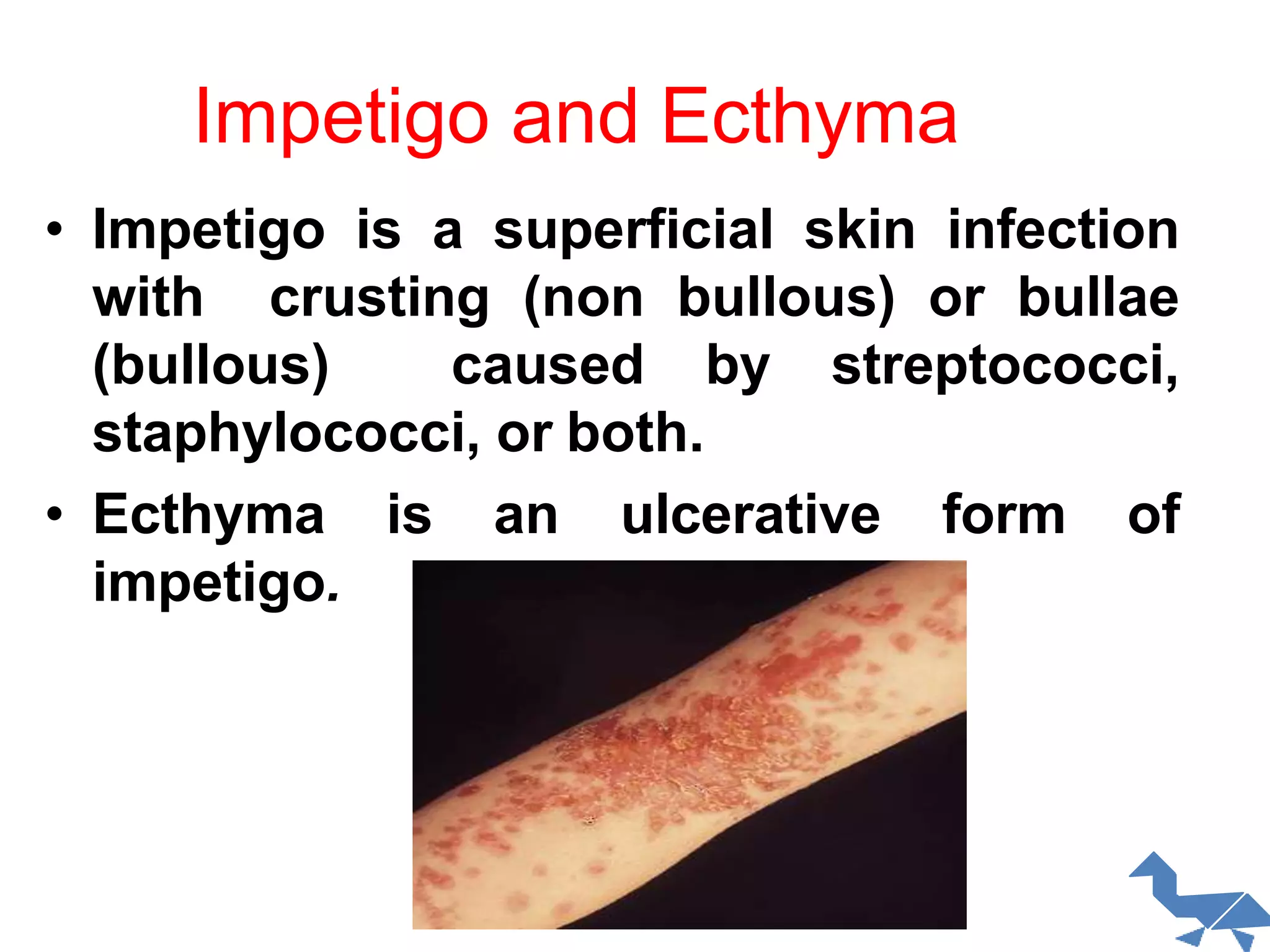
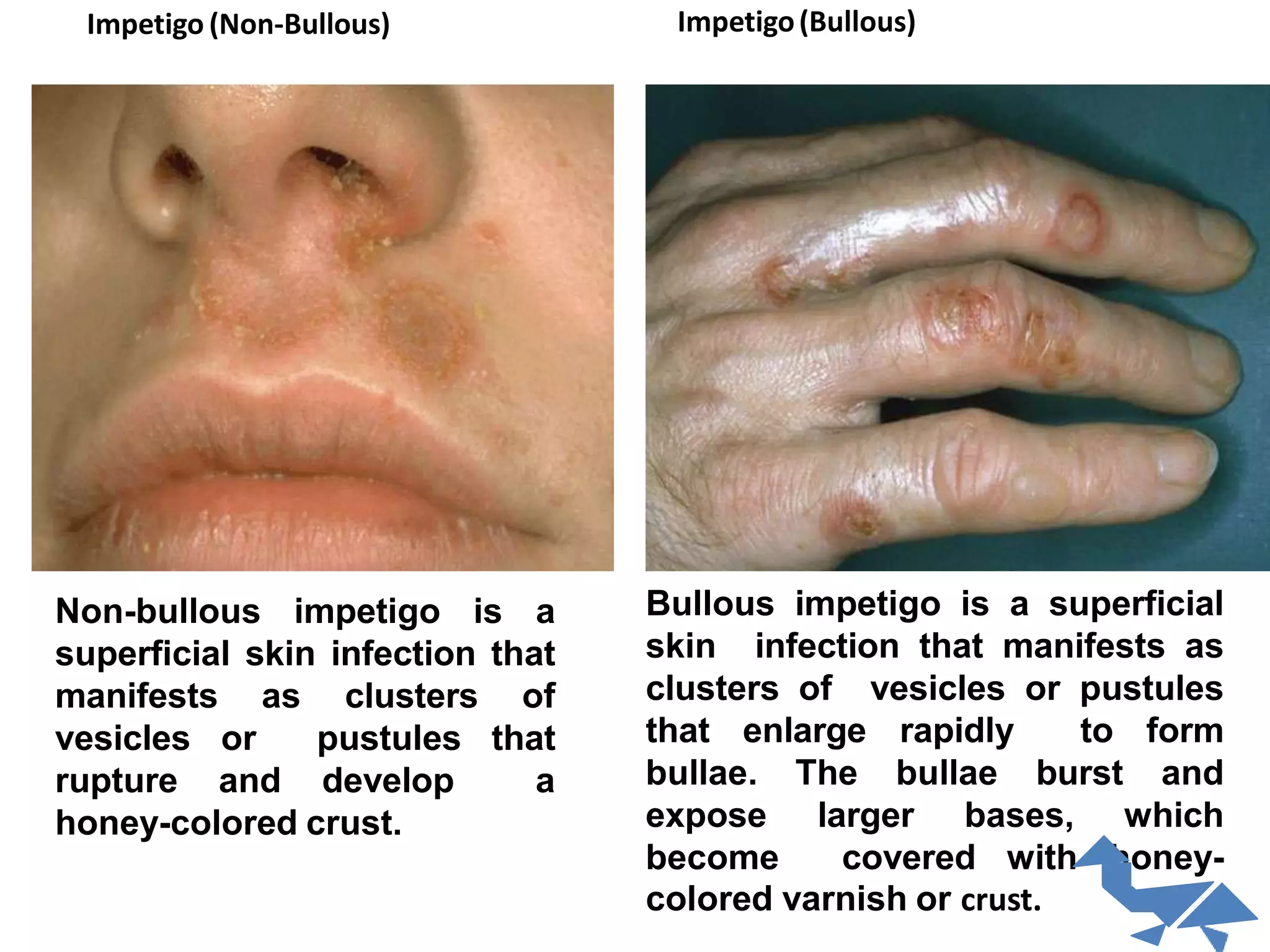
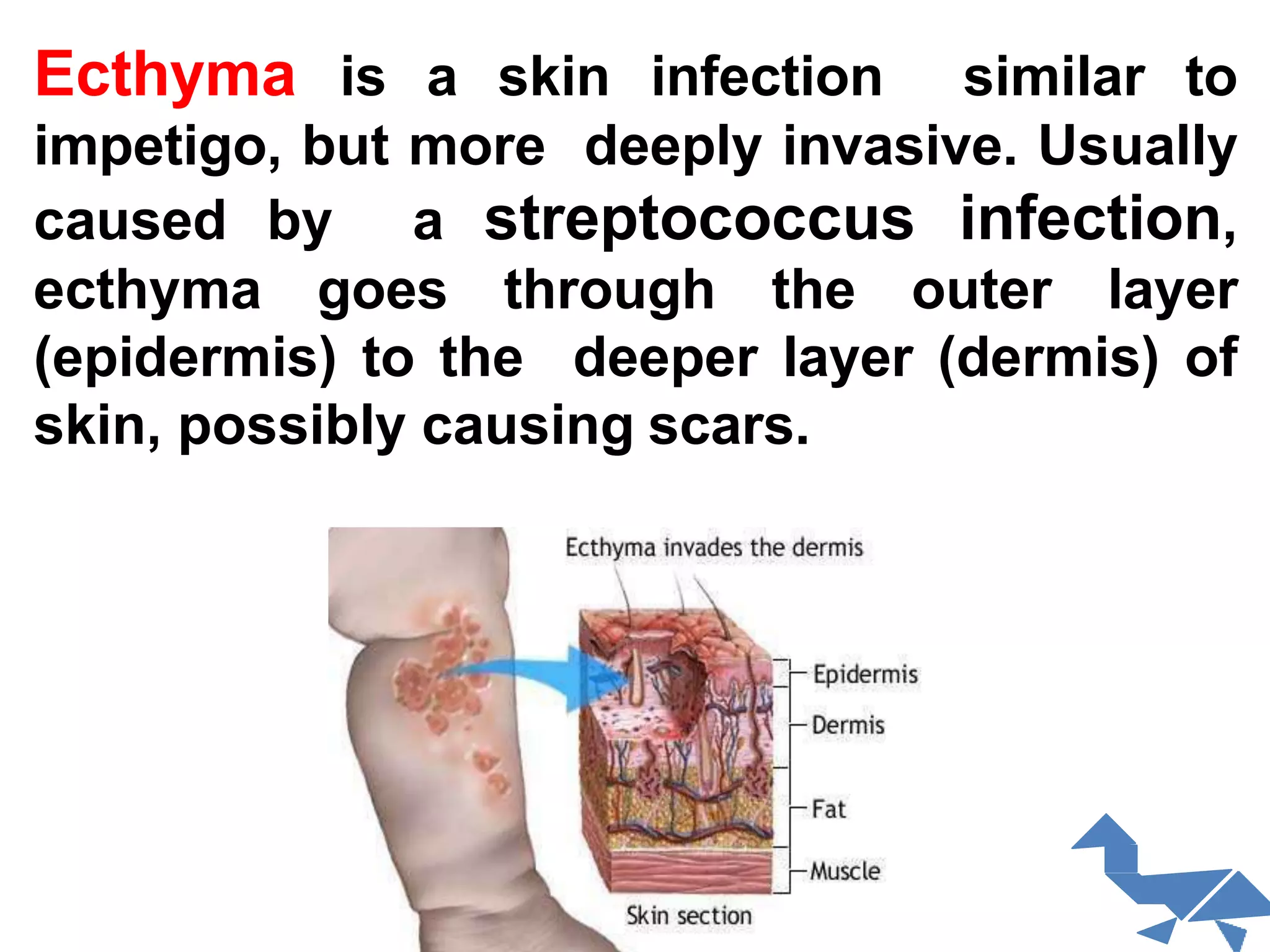
This document provides information about various skin diseases and infections. It begins with an introduction to pathological skin changes and then discusses different types of primary and secondary skin infections. Specific bacterial infections caused by Staphylococcus aureus and group A streptococci are examined. Common skin infections and their symptoms are defined, including impetigo, ecthyma, folliculitis, furuncles, carbuncles, cellulitis, and acne. Diagnosis and treatment of bacterial skin infections is also covered. The document concludes with information about fungal infections such as tinea.