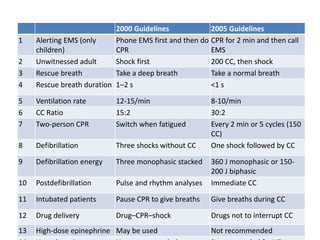
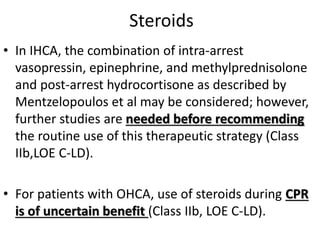
This document summarizes a seminar on the management of cardiac arrest and cardiac arrest survivors. It defines cardiac arrest and discusses mechanisms and causes. It reviews changes to CPR guidelines including a compression to ventilation ratio of 30:2. It discusses factors that affect blood flow during CPR and prognostic factors for poor outcomes. Management strategies are outlined for defibrillation, antiarrhythmic drugs, vasopressors, steroids and extracorporeal CPR. Adjuncts to CPR like oxygen support and monitoring techniques are also summarized.





























































![STATINS
• Reports suggest that, in addition to preventing
vascular events, statins reduce SCD and
appropriate shocks in patients with ICDs.
[Chiu JH, Abdelhadi RH, Chung MK, et al. Effect of statin therapy on risk of ventricular arrhythmia
among patients with coronary artery disease and an implantable cardioverter-defibrillator.
Am J Cardiol. 2005;95(4):490-491. [PMID: 15695135]
• A report from the MADIT II trial found that time-
dependent exposure to statins was associated with a
nearly 30% reduction in appropriate ICD therapy for
VT/VF or cardiac death, after adjustment for other
factors](https://image.slidesharecdn.com/cardiacarrestseminar-181014183230/85/Cardiac-arrest-seminar-67-320.jpg)










![The 2016 American Heart Association (AHA)/American College of Cardiology
(ACC) Clinical Performance and Quality Measures for Prevention of Sudden
Cardiac Death (SCD) propose 10 key measures in the domains of preventative
cardiology, resuscitation/emergency cardiovascular care, heart failure/general
cardiology, and electrophysiology:
1. Smoking cessation intervention in patients who suffered sudden cardiac
arrest (SCA), have ventricular arrhythmias, or are at risk for SCD.
2. Screening for family history of SCD.
3. Screening for asymptomatic left ventricular dysfunction among individuals
who have a strong family history of cardiomyopathy and SCD.
4. Referring for cardiopulmonary resuscitation (CPR) and automatic external
defibrillator (AED) education those family members of patients who are
hospitalized with known cardiovascular conditions that increase the risk of
SCA (any acute myocardial infarction, known heart failure [HF], or
cardiomyopathy).
5. Use of an implantable cardioverter-defibrillator (ICD) for prevention of
SCD in patients with HF and reduced ejection fraction (HFrEF) who have an
anticipated survival of >1 year.](https://image.slidesharecdn.com/cardiacarrestseminar-181014183230/85/Cardiac-arrest-seminar-78-320.jpg)

