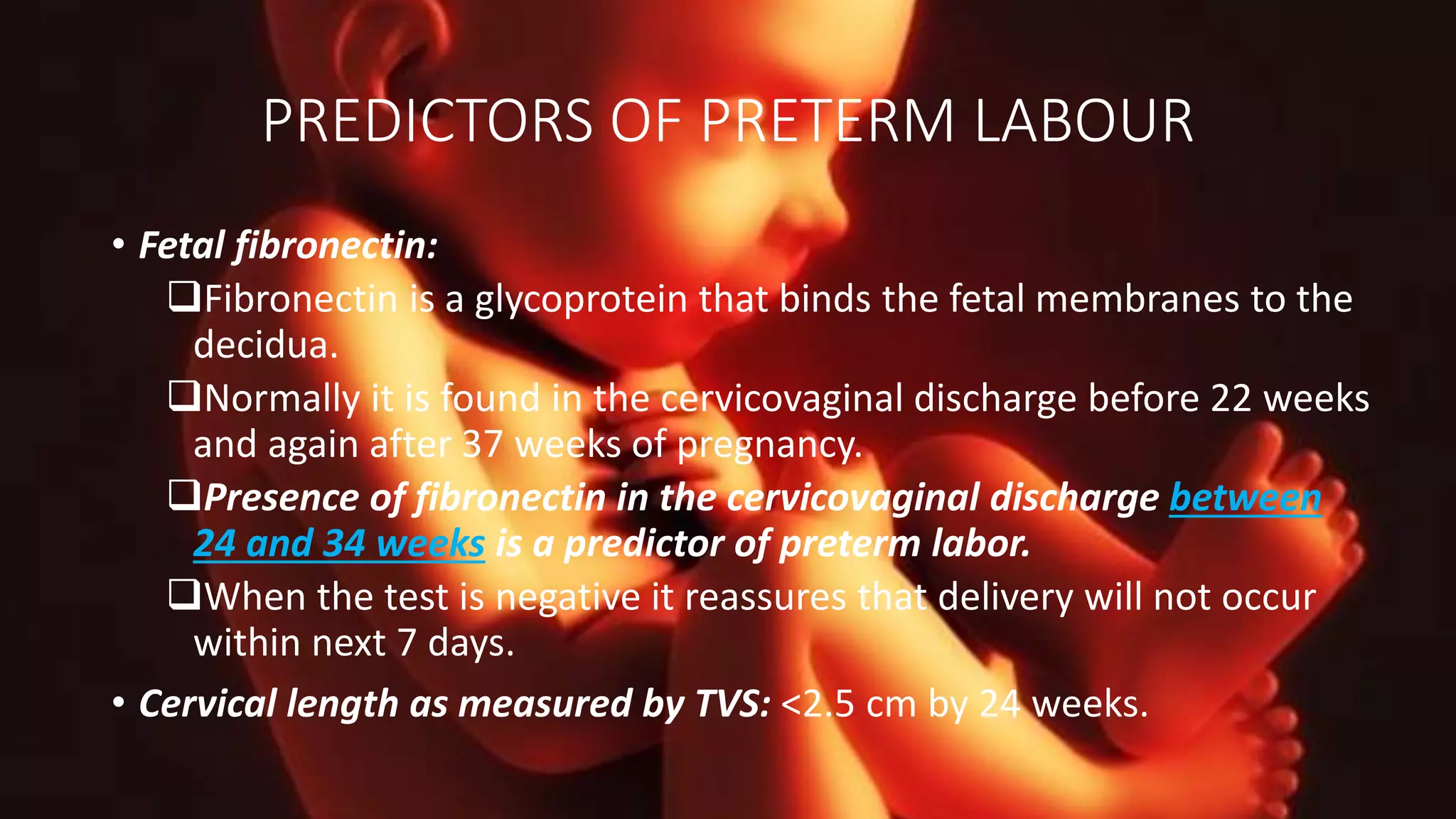
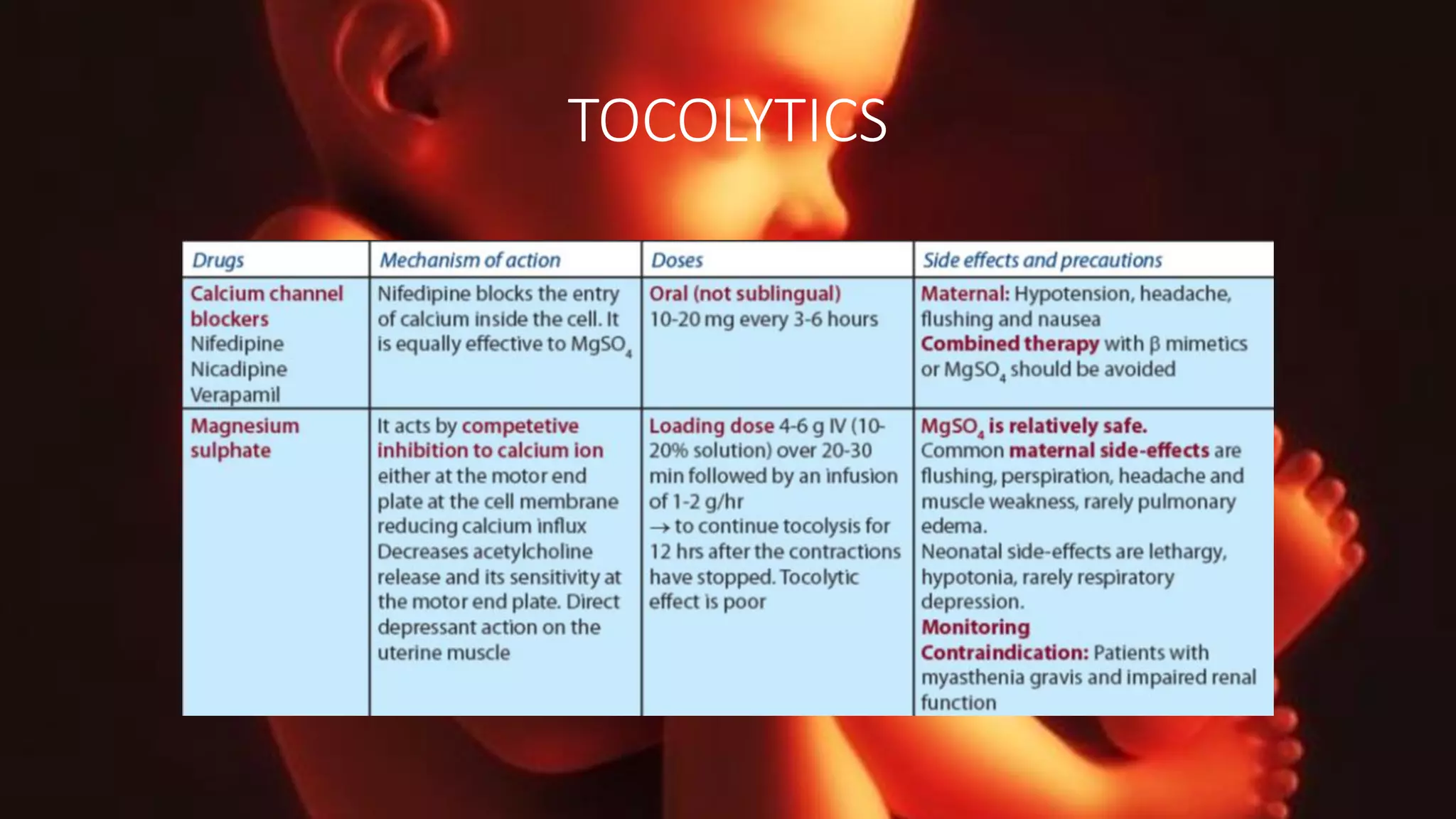
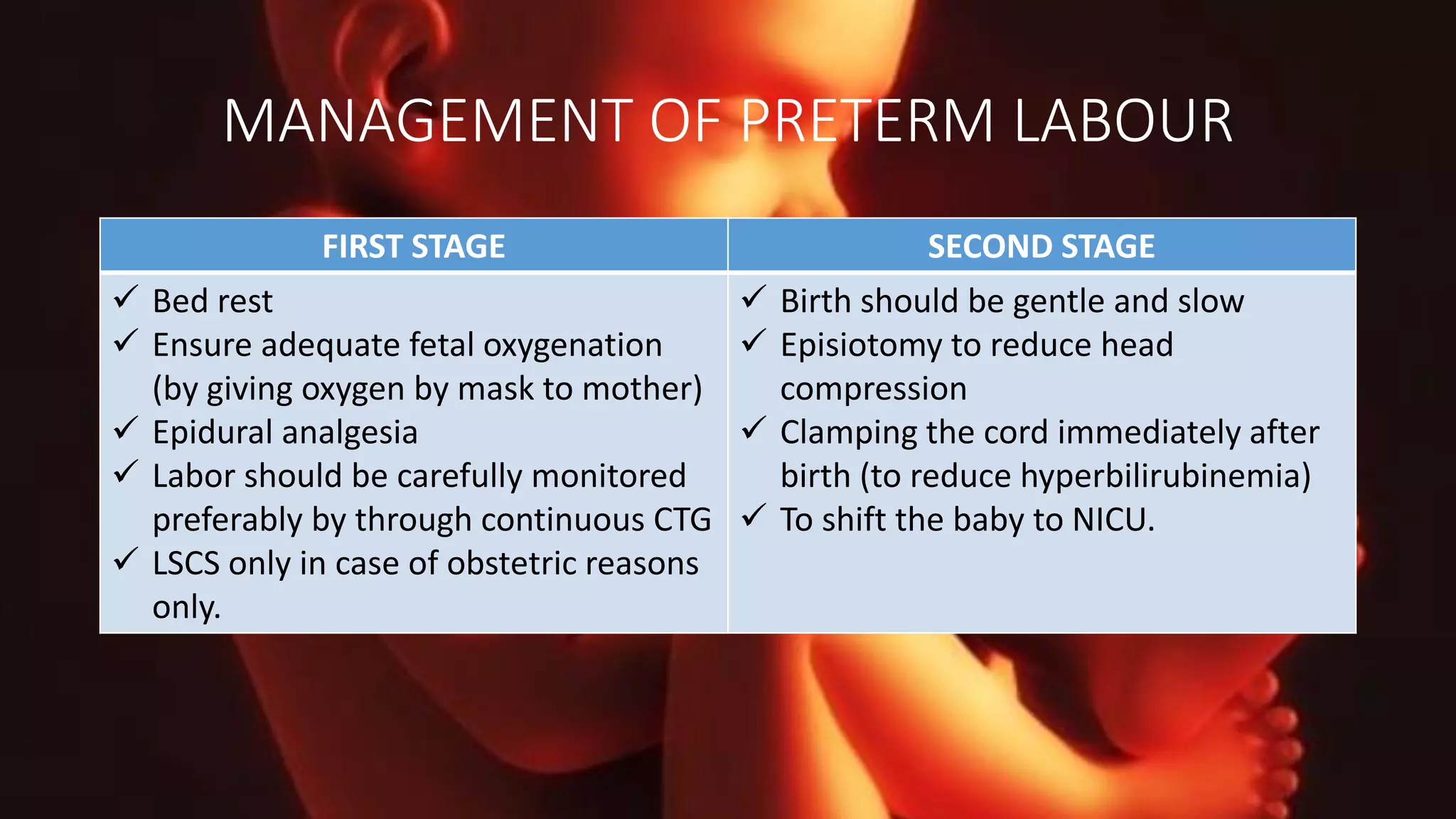
Preterm labor occurs before the 37th week of gestation, with risk factors including previous preterm labor, pre-eclampsia, and multiple pregnancies. Diagnosis relies on regular contractions, cervical dilation, and effacement, while predictors like fetal fibronectin and cervical length aid in assessing risk. Management includes bed rest, hydration, glucocorticoids for fetal lung maturation, and careful monitoring during labor.