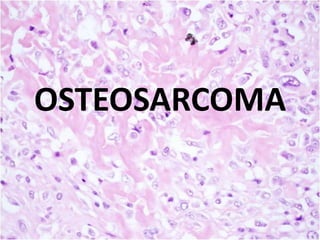
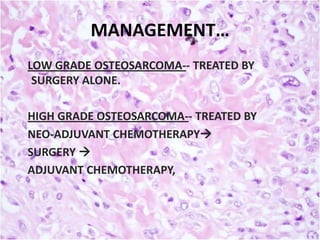
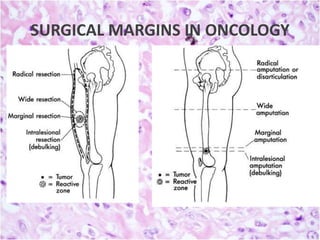
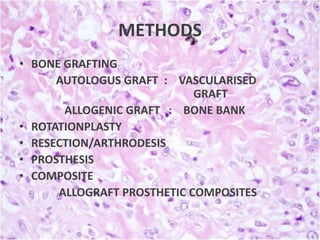
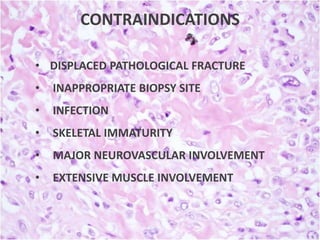
Osteosarcoma is the second-most common primary bone malignancy, primarily affecting adolescents and young adults, with a higher incidence in males. Treatment involves a multidisciplinary approach including chemotherapy, surgery, and occasionally radiotherapy, with limb salvage surgery becoming a standard of care. Prognosis depends on tumor grade, size, and metastasis at diagnosis, with advancements in treatment improving survival rates significantly.