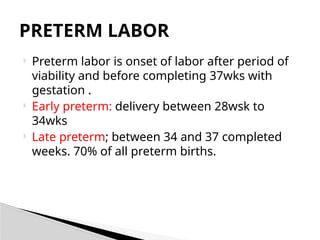
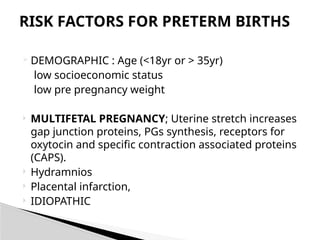
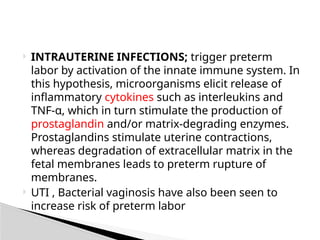
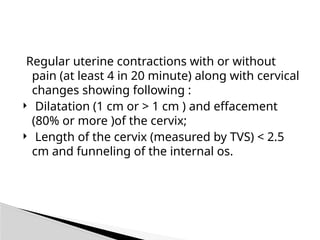
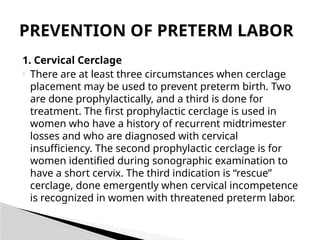
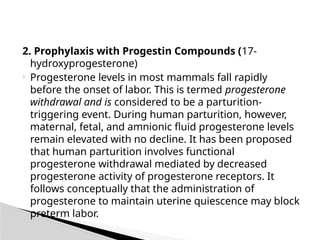
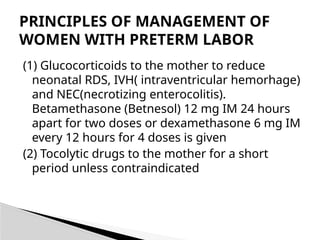
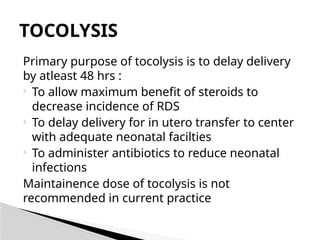
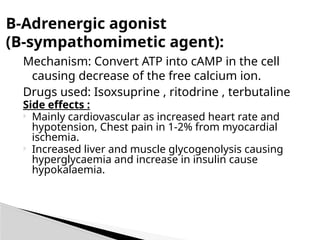
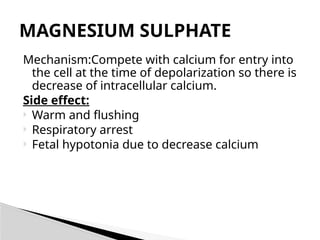
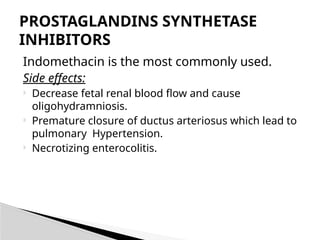
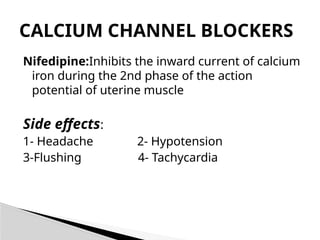
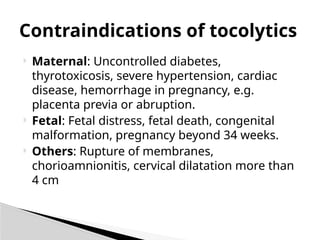
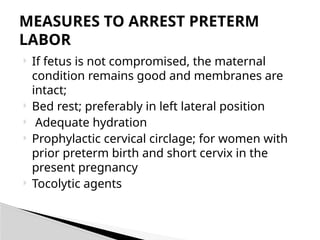
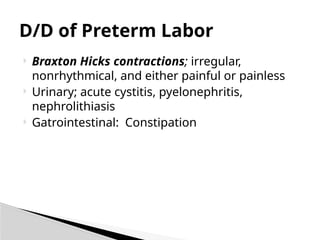
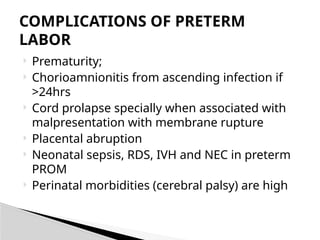
Preterm labor occurs after viability but before 37 weeks of gestation, with causes being multifactorial, including hormonal changes and infection-related inflammation. Risk factors include demographic aspects, previous preterm births, maternal health, and psychological factors, while diagnosis relies on clinical symptoms and ultrasound. Management may involve cerclage, tocolytics, and prophylactic measures to delay delivery and improve neonatal outcomes.