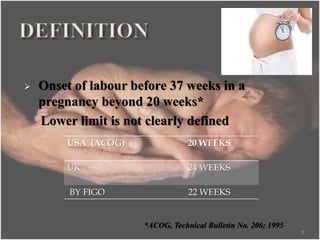
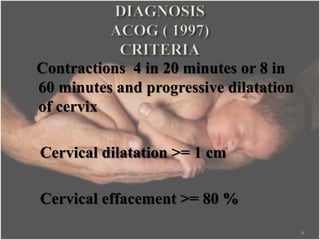
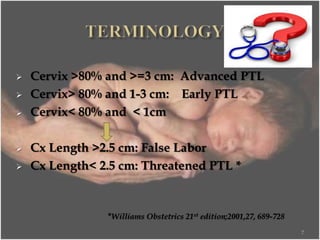
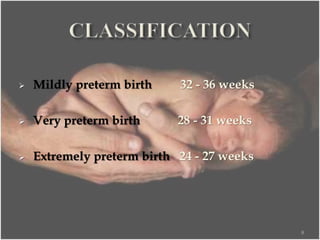
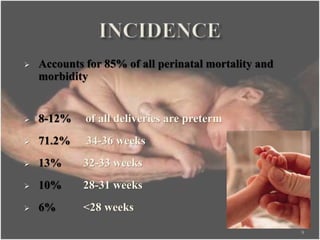
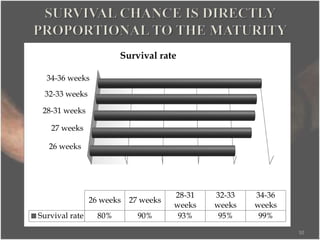
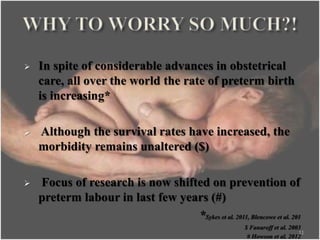
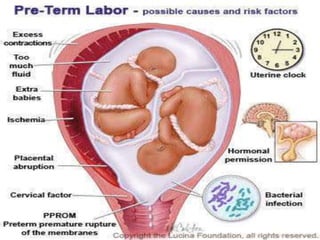
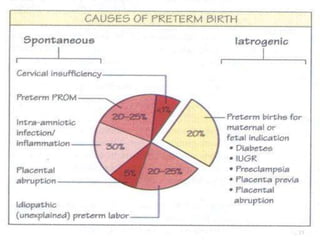
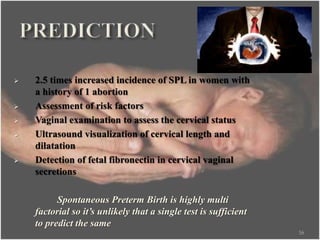
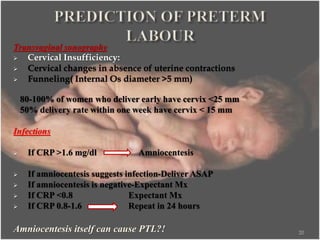
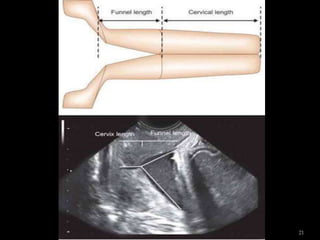
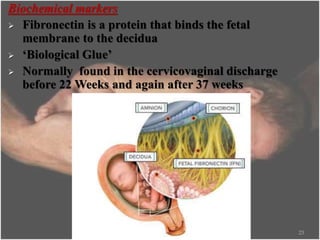
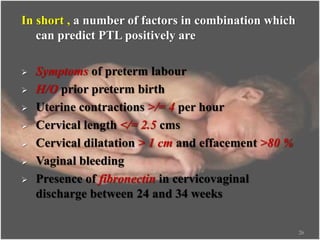
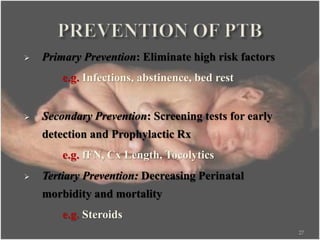
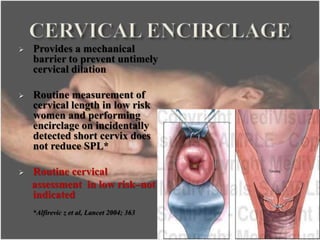
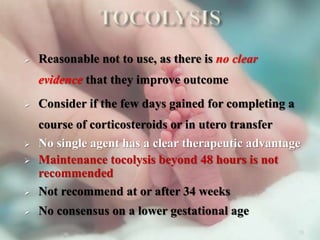
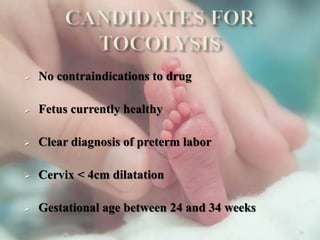
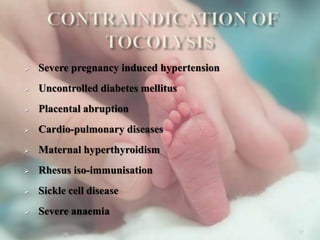
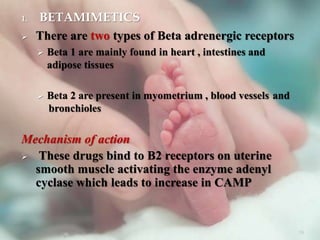
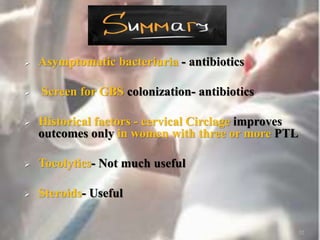
Dr. Kirtan Vyas is an assistant professor who has numerous qualifications and accomplishments. He has published in international journals, presented at conferences, and held various organizational roles. The document discusses preterm labor (PTL), defining it as labor before 37 weeks of pregnancy. It outlines the significance and risk factors of PTL and describes the initial evaluation, management, and potential neonatal complications of PTL. Evaluation includes examination, ultrasound, and biochemical markers to assess the status of the cervix and predict the likelihood of preterm delivery."