The document discusses potassium metabolism and disorders of potassium levels. It covers:
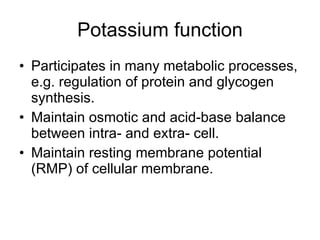
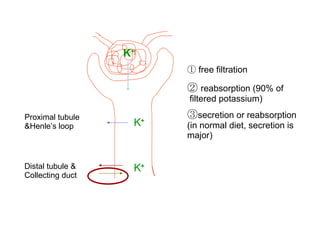
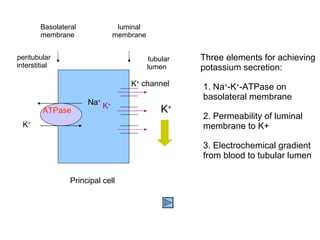
1) Normal potassium metabolism and regulation by the kidneys, factors that influence renal secretion/excretion.
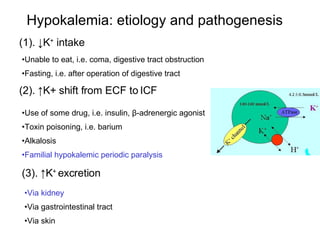
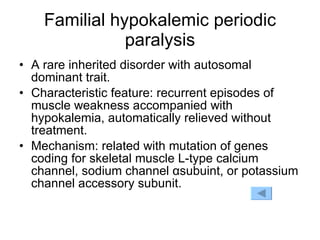
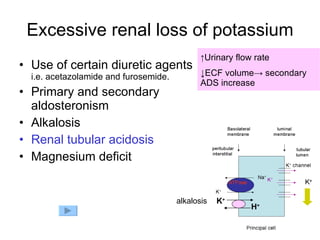
2) Causes and pathophysiology of hypokalemia and hyperkalemia, including excessive renal/gastrointestinal loss or intake, shifts between intracellular/extracellular fluid.
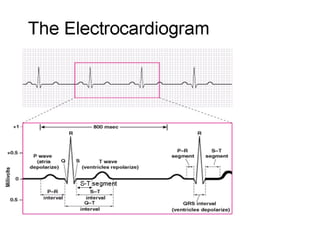
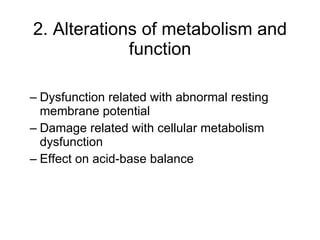
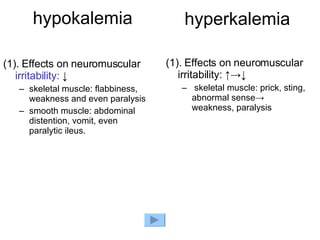
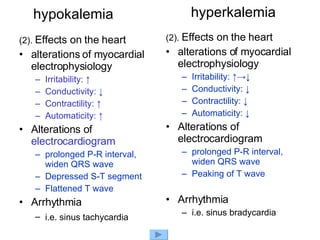
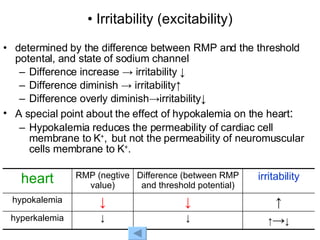
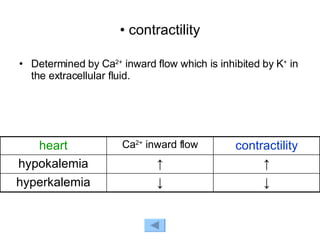
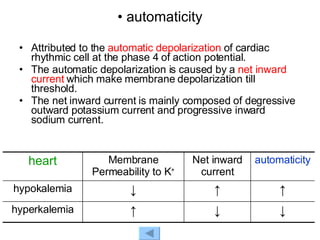
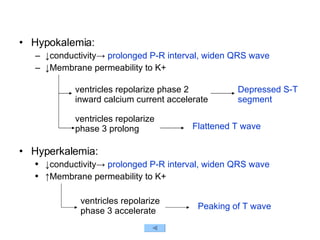
3) Effects of abnormal potassium levels on neuromuscular and cardiac function, including changes in membrane potential and electrical activity.

![K + Na + ATPase K + H + K + channel 140-160 mmol/L 4.2±0.3mmol/L 50-200mmol/day K + ingestion Kidney colon skin (90%) insulin β-adrenergic agonist ECF [K + ] K + : 50-55mmol/kg B.W toxin (Ba) acid-base state Pump-leak](https://image.slidesharecdn.com/potassium-imbalance-1208278900012672-8/85/Potassium-Imbalance-4-320.jpg)
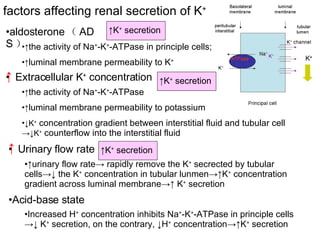
![K + Na + ATPase K + H + K + channel 140-160 mmol/L 4.2±0.3mmol/L 50-200mmol K + ingestion Kidney colon skin (90%) insulin β-adrenergic agonist ECF [K + ] 50-55mmol/kg B.W ADS ECF K + concentration Urinary flow rate acid-base state toxin drug acid-base state](https://image.slidesharecdn.com/potassium-imbalance-1208278900012672-8/85/Potassium-Imbalance-8-320.jpg)







![Permeability RMP negative value ↓ -> ↓ i.e. normal -90mv -> -70mv Extracellular K + concentration [K + ] e RMP negative value ↓ -> ↑ ↑ -> ↓ Electrical gradient Chemical gradient K + 140-160mmmol/L 4.2±0.3mmol/L Resting membrane potential (RMP) Excitable cell Cell membrane permeability to K + K + transmembrane concentration gradient - - - - - + + + + + Na + ATPase RMP ≈ ﹣ 59.5lg Intracellular K + concentration extracellular K + concentration](https://image.slidesharecdn.com/potassium-imbalance-1208278900012672-8/85/Potassium-Imbalance-21-320.jpg)





![hypokalemia (3). Effects on acid-base balance alkalosis Paradoxical aciduria (3). Effects on acid-base balance acidosis Paradoxical alkaline urine hyperkalemia ↓[K + ] ECF H + -K + exchange ↓[H + ] ECF ↑[H + ] ICF ↑Renal excretion of H + aciduria K + shift out of cells H + shift into cells alkalosis (Paradoxical aciduria) ↑[K + ] ECF H + -K + exchange ↑[H + ] ECF ↓[H + ] ICF ↓Renal excretion of H + Alkaline urine K + shift into cells H + shift out of cells acidosis (Paradoxical alkaline urine)](https://image.slidesharecdn.com/potassium-imbalance-1208278900012672-8/85/Potassium-Imbalance-33-320.jpg)