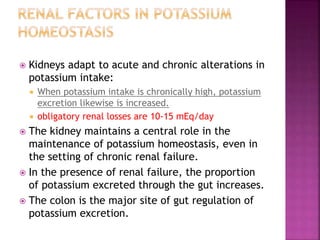
The document provides a comprehensive overview of hypokalemia, its causes, symptoms, and management strategies. It details the physiological role of potassium, factors influencing its homeostasis, and the common mechanisms leading to its deficiency. Treatment approaches include dietary supplementation, addressing underlying causes, and careful monitoring of potassium levels, especially in cases of severe hypokalemia.






























![ Eating disorders (incidence of 4.6-19.7% in an
outpatient setting)
AIDS (23.1% of hospitalized patients)
Alcoholism (incidence reportedly as high as
12.6% [33] in the inpatient setting), likely from
a hypomagnesemia-induced decrease in
tubular reabsorption of potassium
Bariatric surgery](https://image.slidesharecdn.com/potassiummanagement-150917112458-lva1-app6892/85/hypokalemia-diagnosis-and-management-33-320.jpg)




