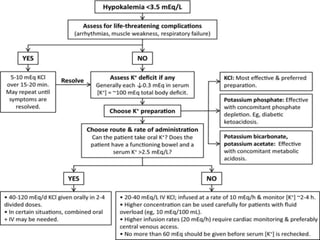
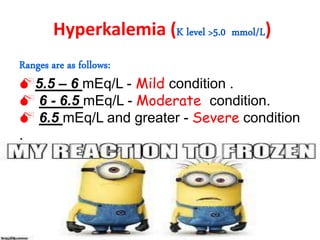
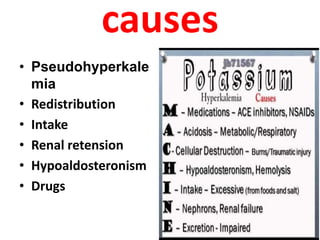
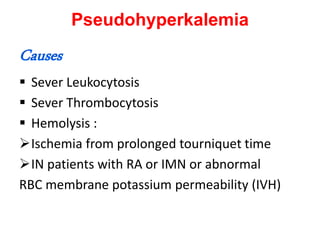
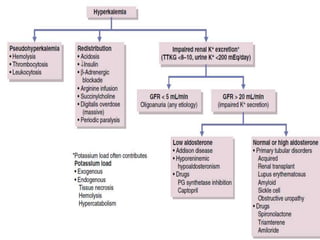
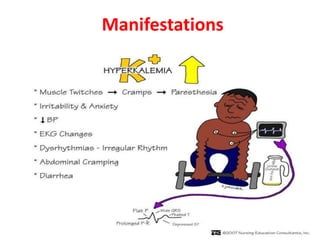
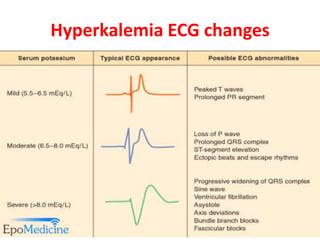
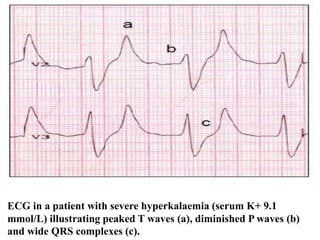
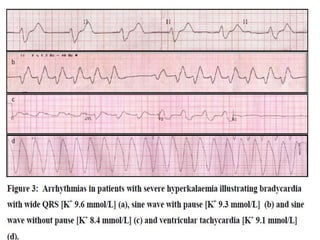
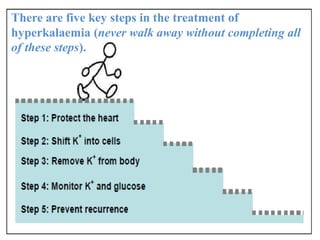
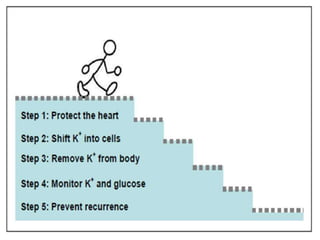
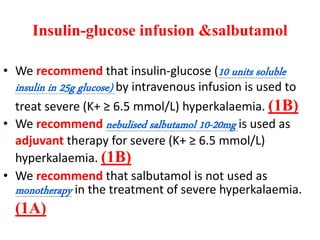
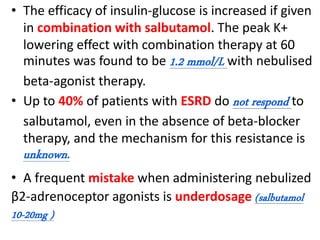
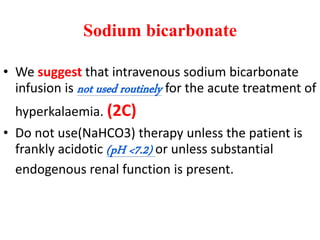
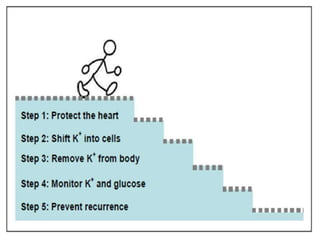
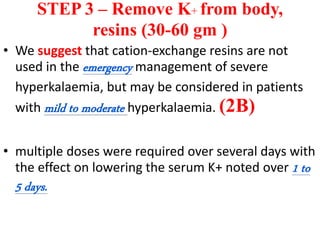
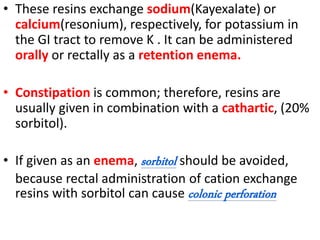
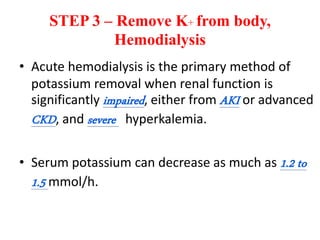
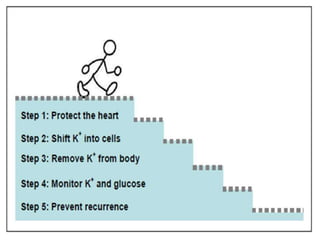
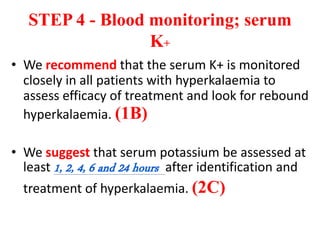
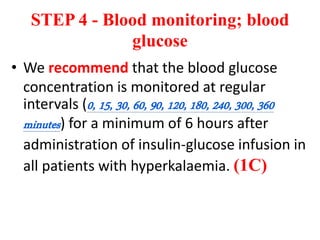
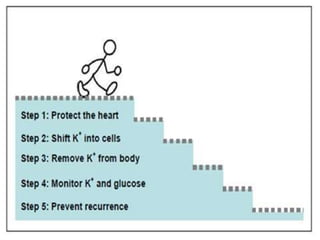
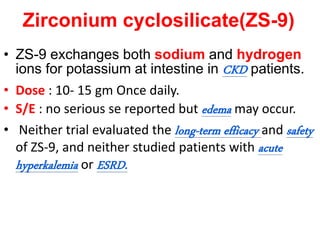
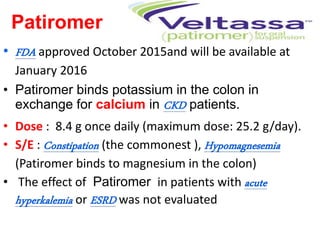
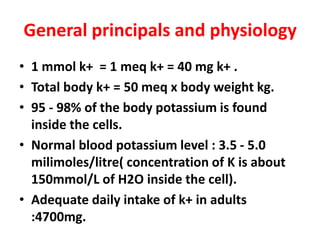
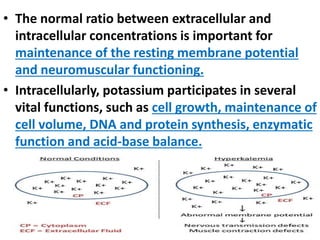
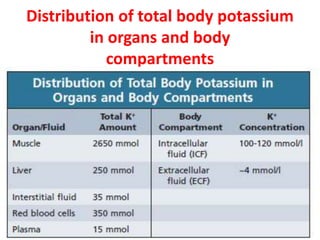
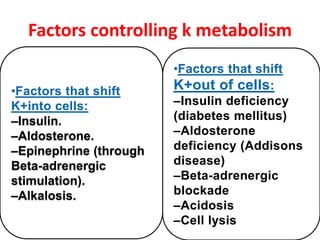
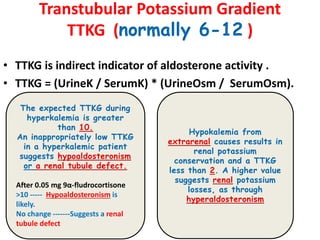
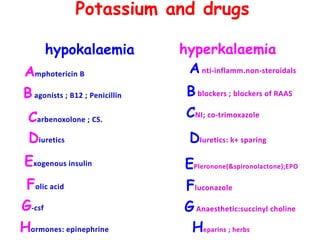
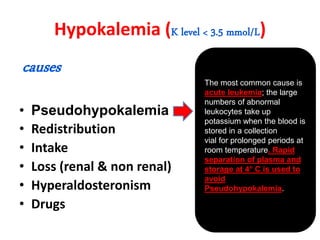
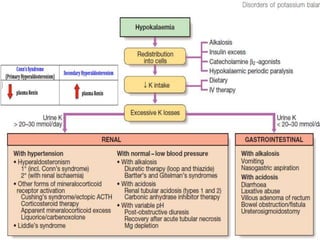
The document outlines potassium disorders, including hypokalemia and hyperkalemia, discussing their causes, manifestations, diagnostic approaches, and management strategies. It emphasizes the importance of potassium for cellular functions and provides insights into the physiological principles governing potassium metabolism. Additionally, it reviews treatment protocols for both conditions, including pharmacological interventions and dietary considerations, along with recent updates on new potassium-binding agents.

![• Every 1mmEq/ L [K+] depletion = 10 % Reduction
of total body K+store.
• [Total body K+content = 50mEq/ KG]
• For a 60 kg person, total body K+store = 60 x 50=
3000 mEq. Therefore, 1 mEq/ L [K+] depletion =
3000 x 10% = 300 mEq. = Total K+ deficit.
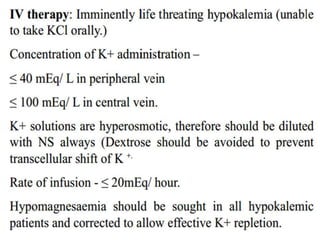
• Oral or enteral administration is preferred if the
patient can take oral medication and has normal GI
tract function. Acute hyperkalemia is highly
unusual when potassium is given orally.
• parenteral KCl should be administered in dextrose-
free solutions.](https://image.slidesharecdn.com/potassiumdisorders-160323052923/85/Potassium-disorders-comprehensive-practical-approach-20-320.jpg)