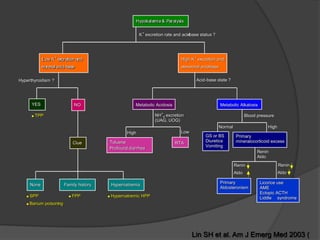
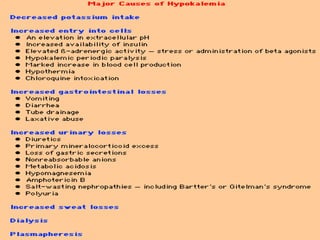
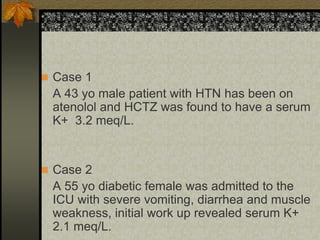
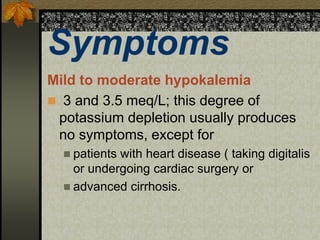
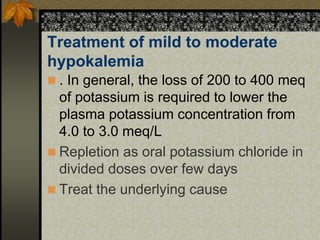
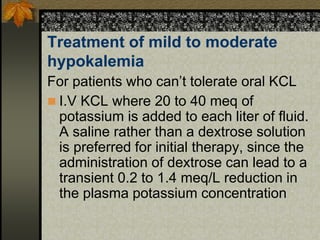
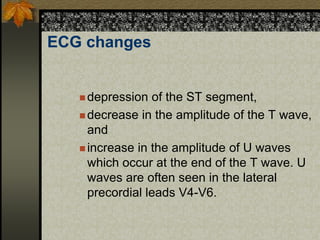
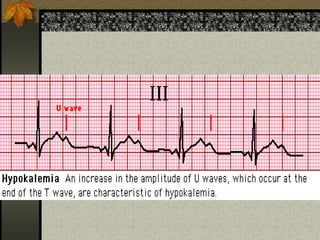
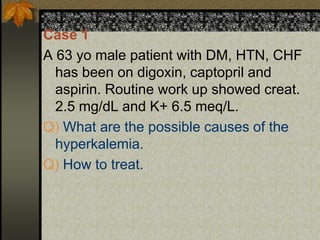
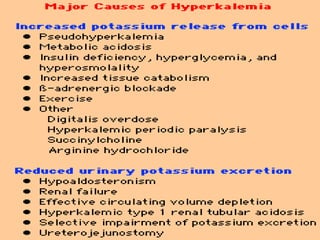
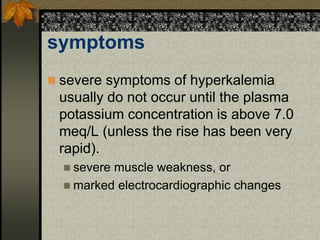
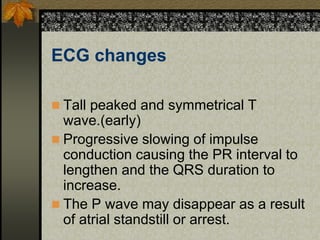
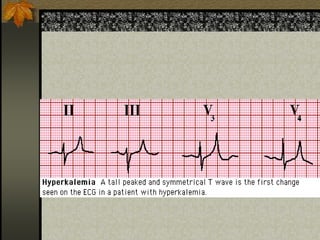
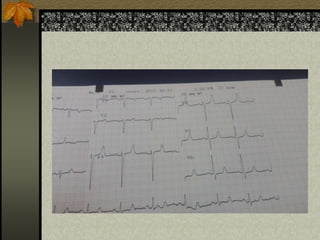
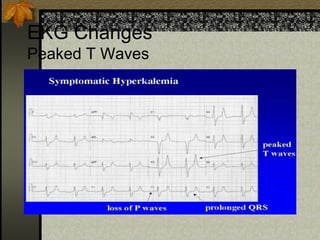
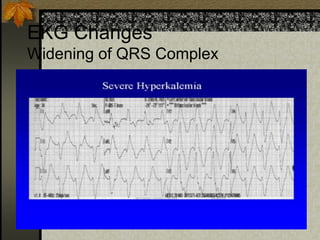
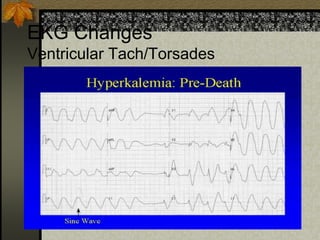
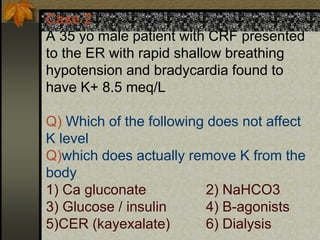
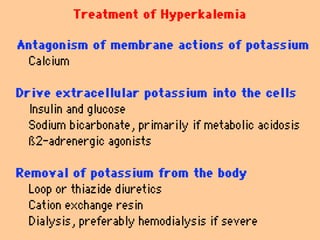
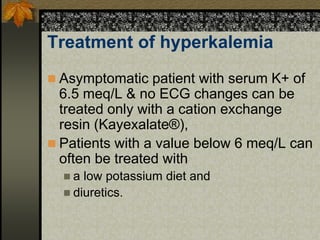
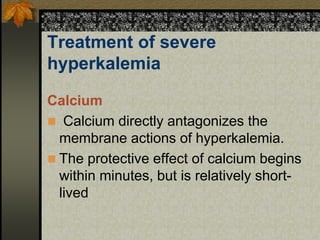
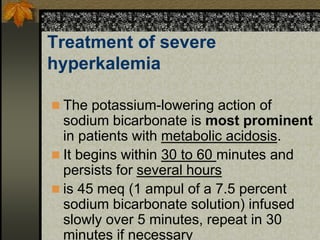
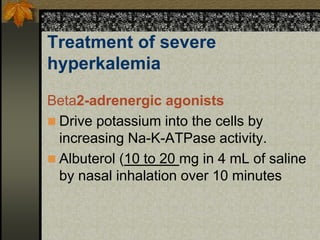
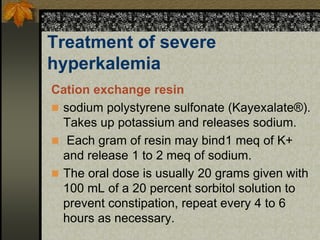
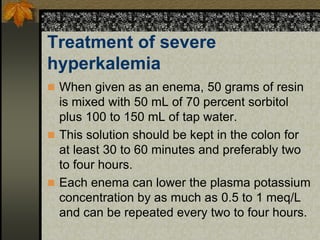
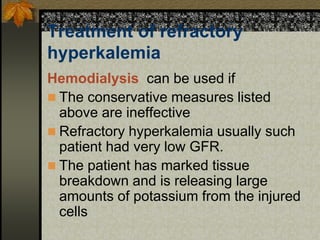
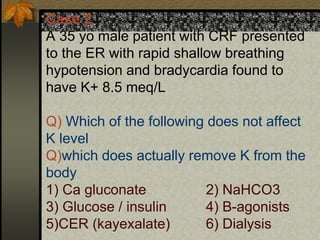
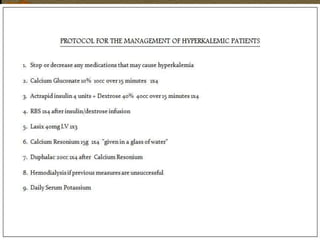
The document discusses electrolyte disturbances, focusing on hypokalemia and hyperkalemia, their definitions, causes, symptoms, and treatment options. Hypokalemia is characterized by low serum potassium levels and can present with symptoms like muscle weakness and ECG changes, while hyperkalemia involves elevated potassium levels and can lead to severe cardiac issues. Treatment approaches vary based on severity, ranging from oral potassium supplementation to intravenous administration and interventions to stabilize cardiac function.