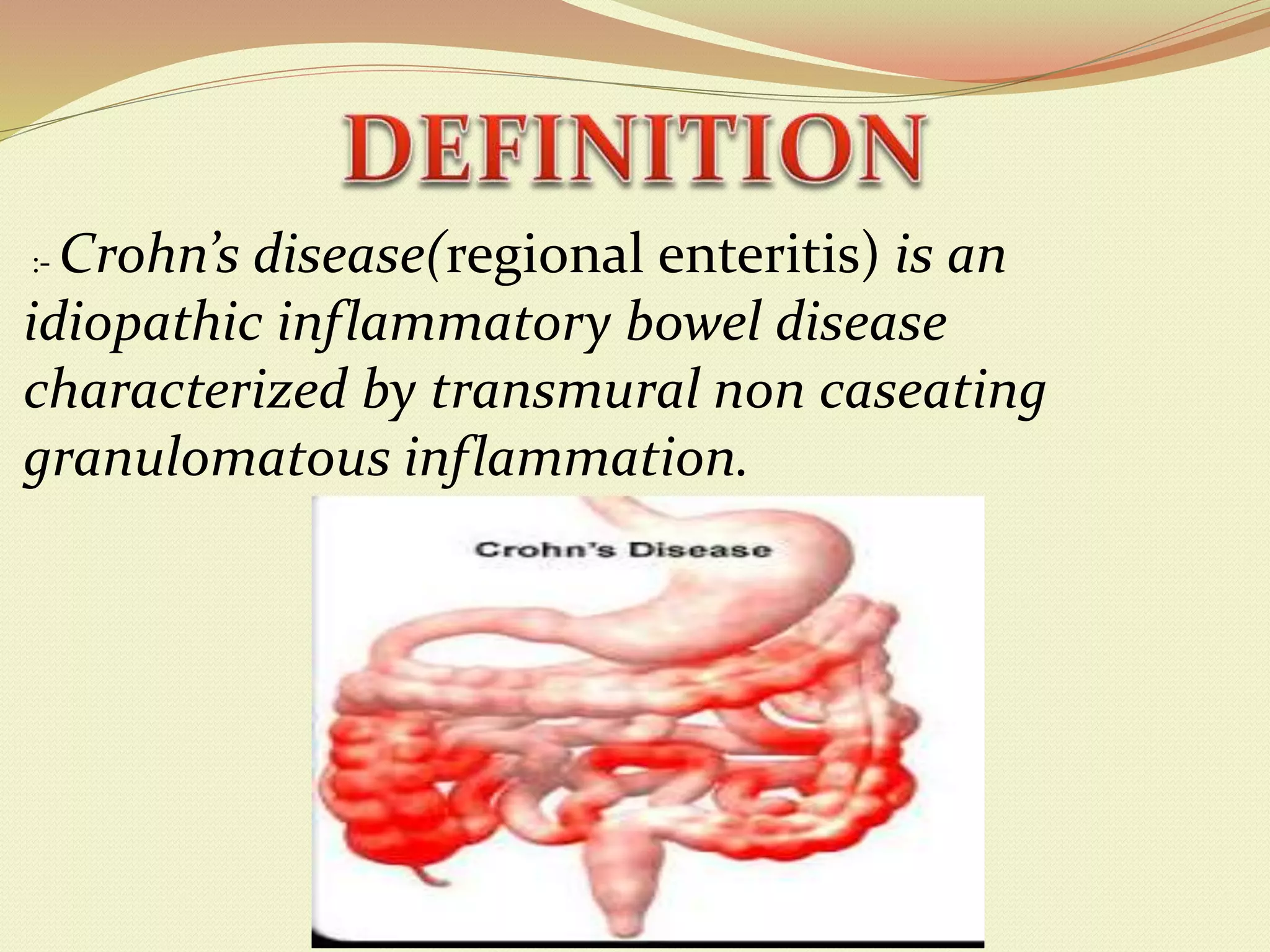
Crohn's disease is an idiopathic inflammatory bowel disease characterized by transmural inflammation that can occur anywhere along the gastrointestinal tract from mouth to anus. It most commonly affects the terminal ileum and causes symptoms like diarrhea, abdominal pain, and weight loss. While the exact causes are unknown, it is believed to involve genetic susceptibility and an abnormal immune response triggered by environmental factors. Diagnosis involves examinations like colonoscopy, CT, MRI and blood tests. Treatment focuses on reducing inflammation using medications like antibiotics, aminosalicylates, corticosteroids, immunomodulators, and biologics. Complications can be intestinal, systemic, or postoperative.