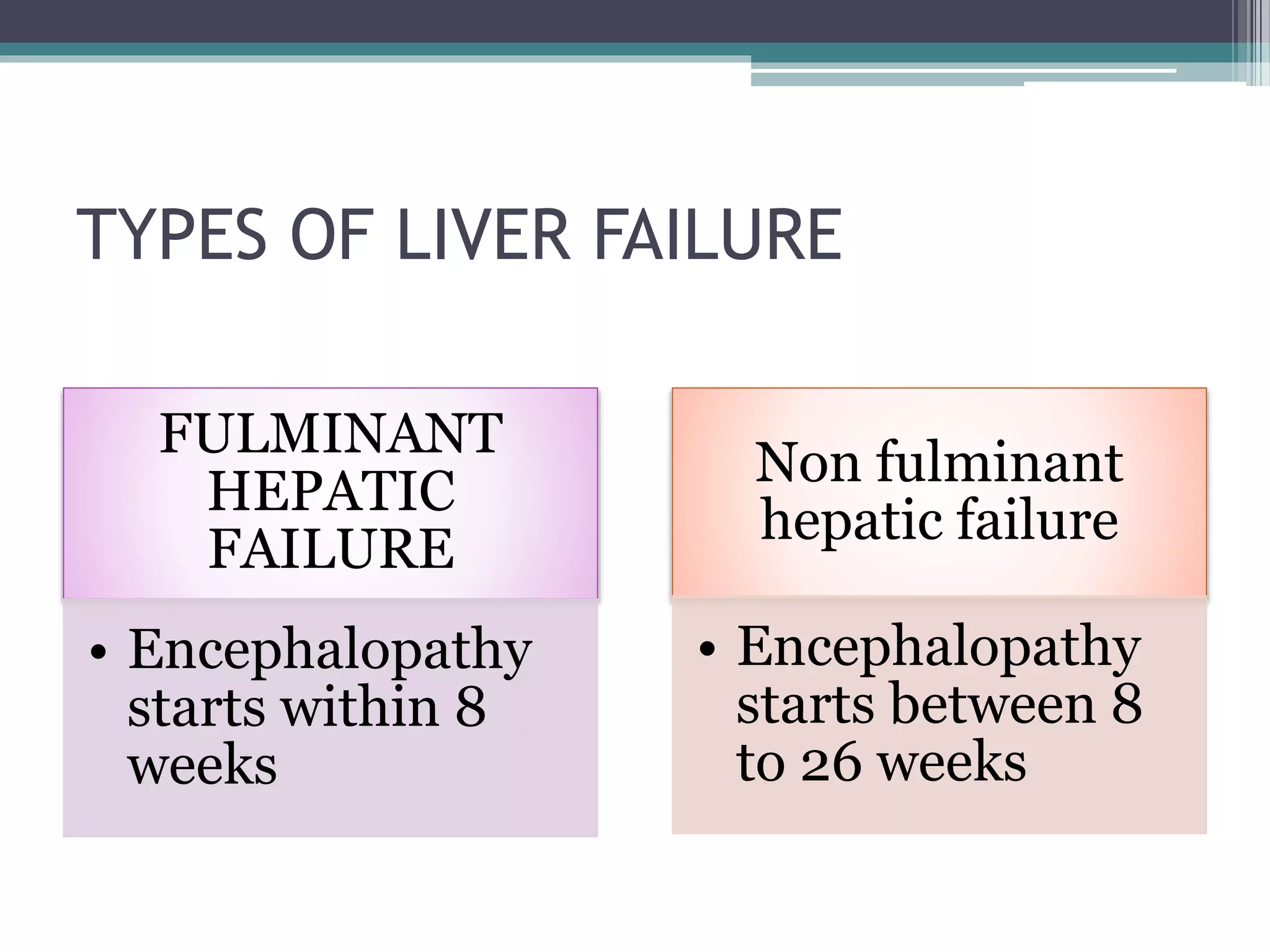
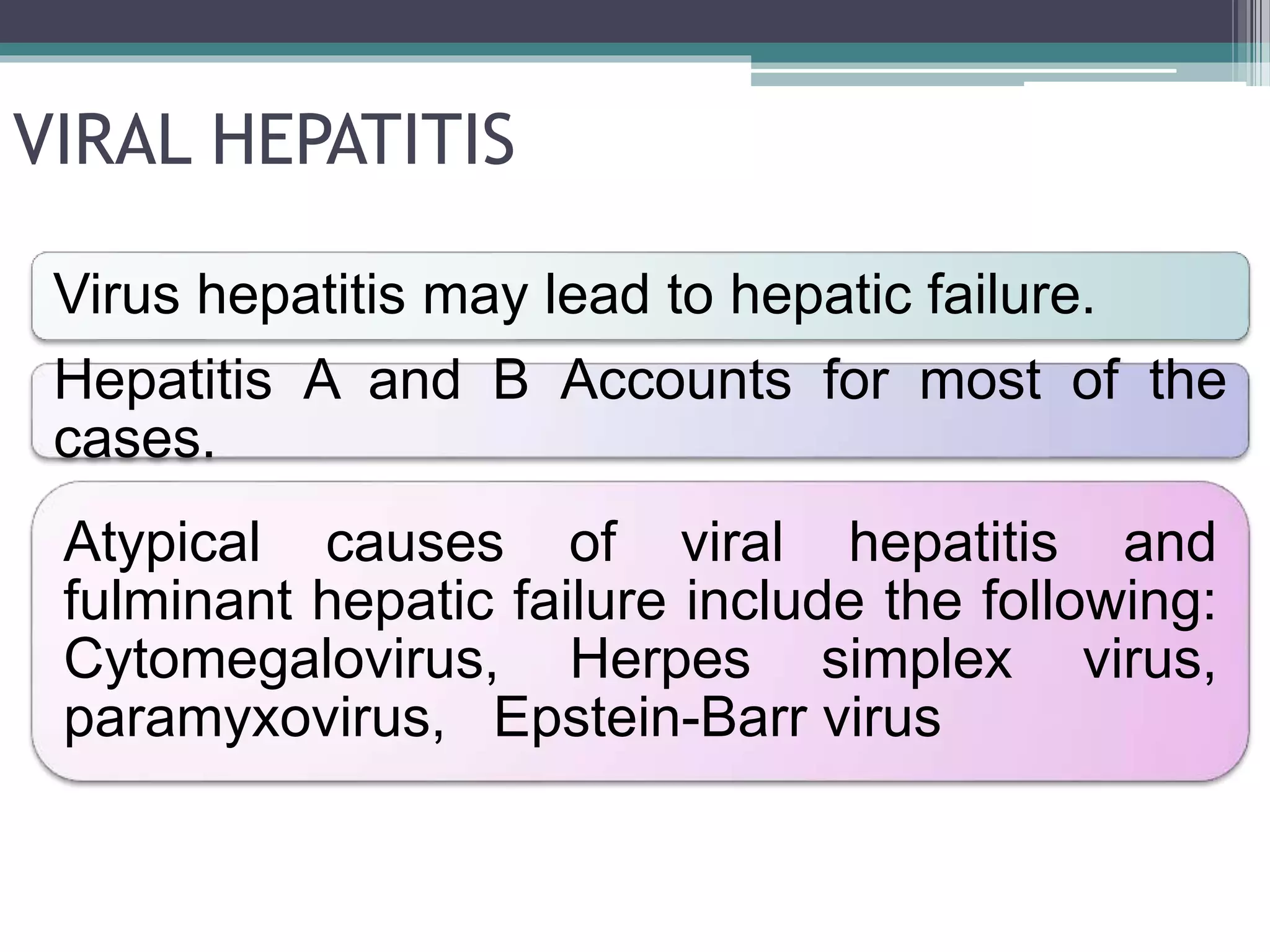
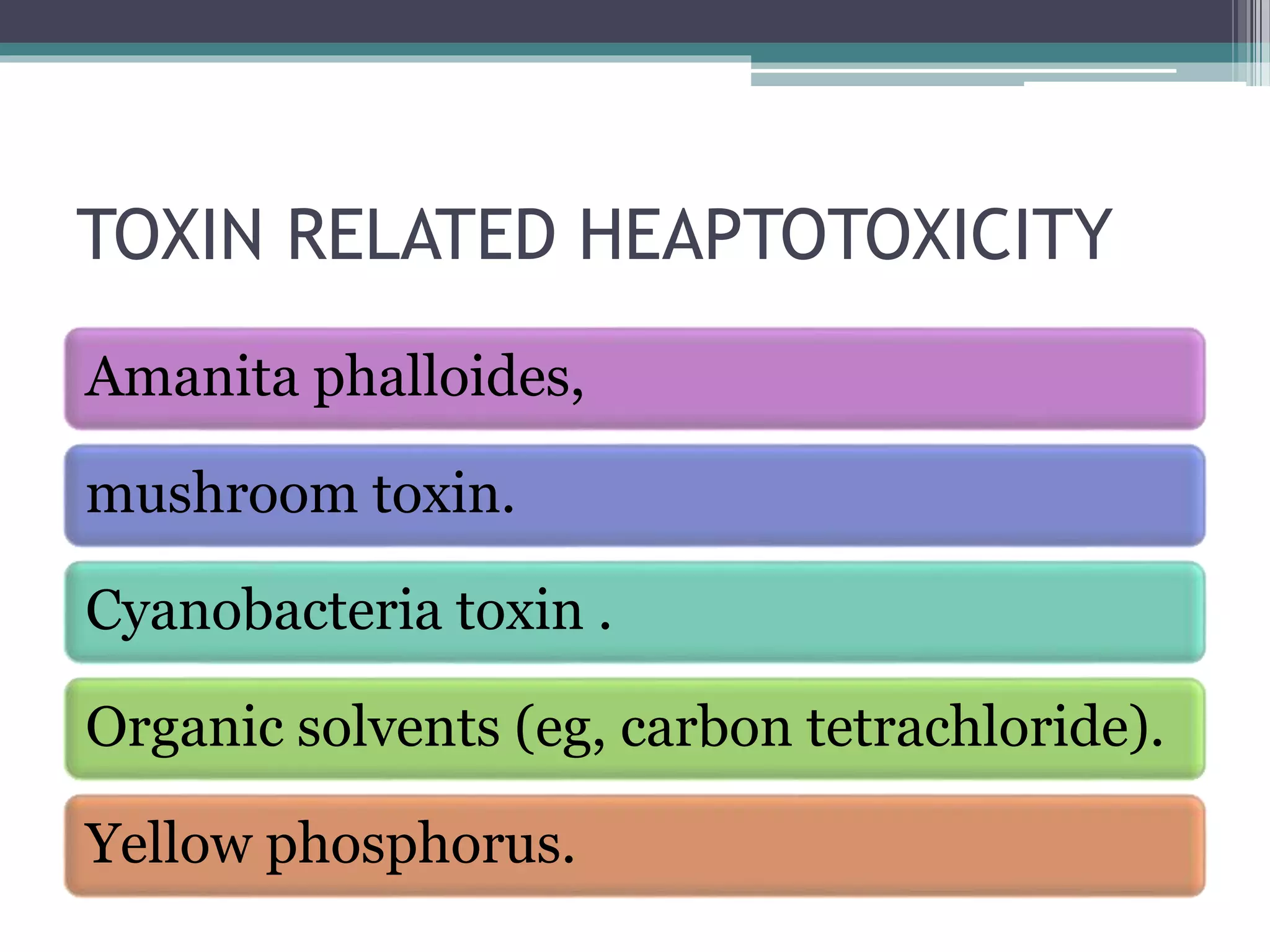
Liver failure occurs when the liver rapidly loses its ability to function, resulting in mental status changes and coagulation abnormalities. It can be caused by viral hepatitis, drug toxicity, toxins, vascular issues, or metabolic diseases. Acute liver failure presents as a sudden onset of severe liver injury in someone without pre-existing liver disease. It requires emergency treatment and may necessitate a liver transplant if liver function cannot be reversed. Management involves supportive care, medications to treat complications, and sometimes a liver transplant.