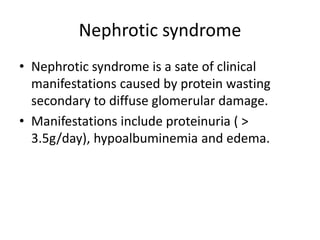
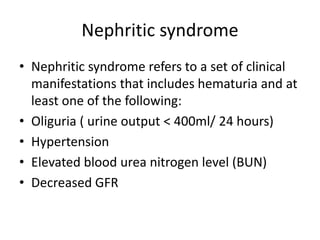
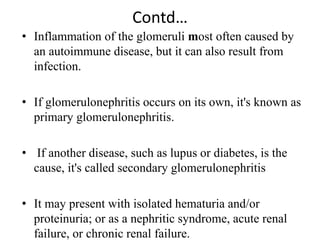
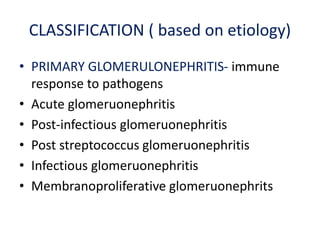
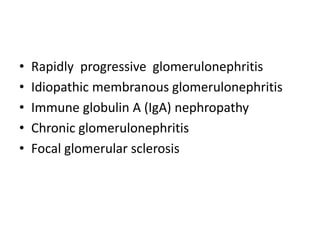
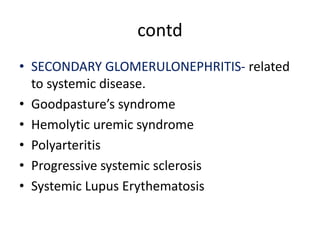
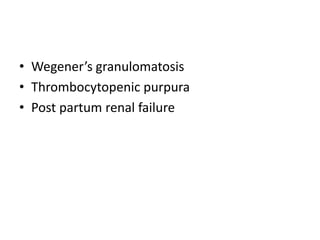
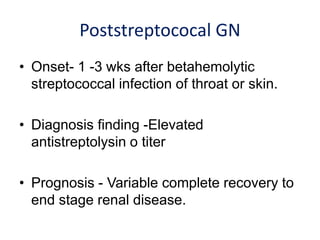
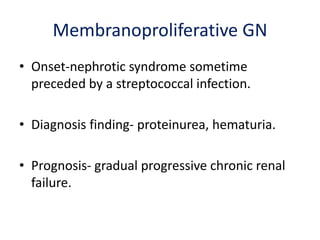
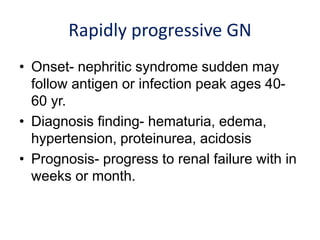
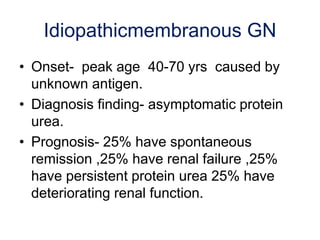
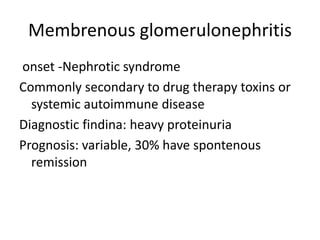
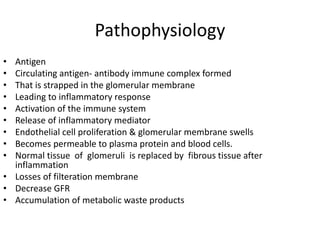
Glomerulonephritis is an inflammation of the glomerular capillaries in the kidney. It can be caused by an immunological reaction that results in proliferative and inflammatory changes to the glomerular structure. Antigen-antibody complexes form in the blood and become trapped in the glomerular capillaries, inducing an inflammatory response. Glomerulonephritis can present as either a nephrotic syndrome with heavy proteinuria and edema, or a nephritic syndrome with hematuria and decreased kidney function. Treatment involves managing symptoms, preserving kidney function, and treating complications early.