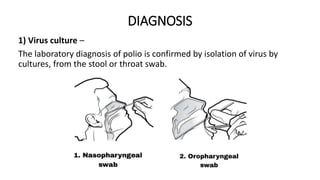
1) Poliomyelitis is an infectious disease caused by the poliovirus that affects the spinal cord. It commonly affects children under 5 years old and can cause paralysis.
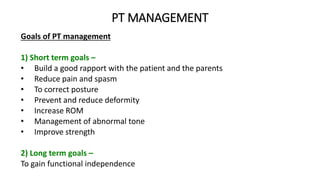
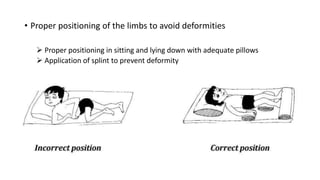
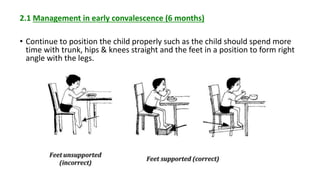
2) Physical therapy management for poliomyelitis involves range of motion exercises, positioning, splinting, and strengthening to prevent deformities and improve function. Surgical procedures like tendon lengthening or transfers may be used for severe contractures.
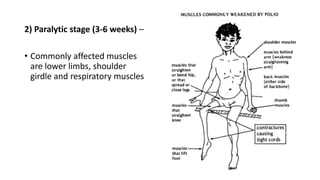
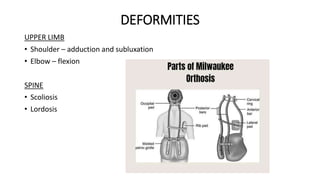
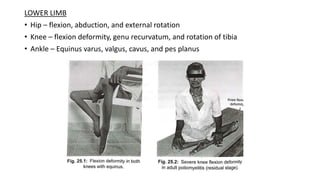
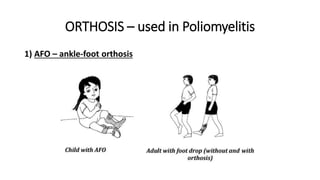
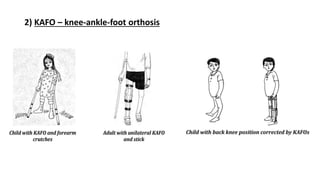
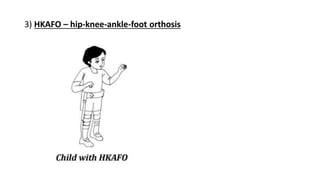
3) Common deformities from polio include shoulder adduction, elbow flexion, scoliosis, hip flexion, and knee flexion. Orthoses like AFOs, KAFOs, and HKAFOs can help correct deformities and improve gait.