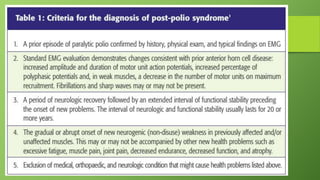
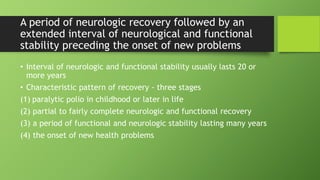
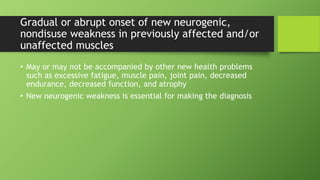
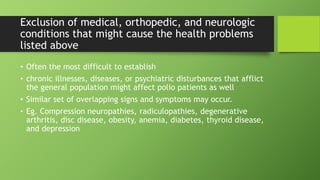
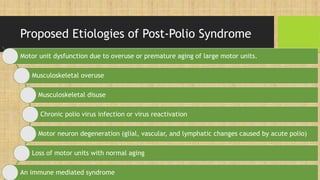
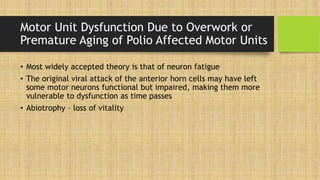
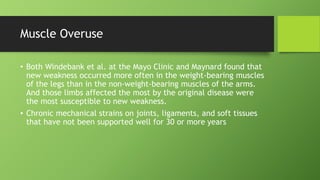
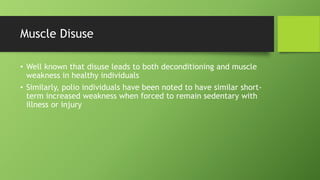
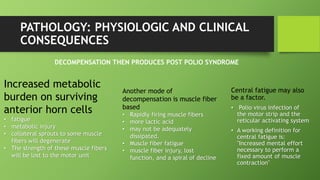
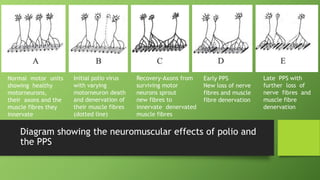
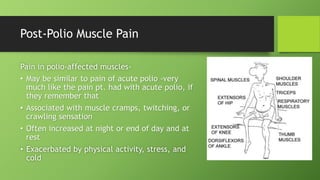
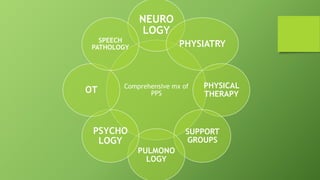
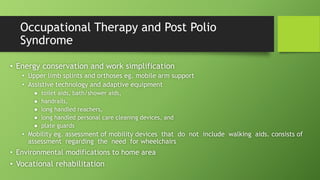
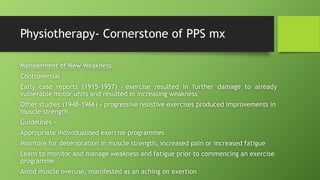
Post polio syndrome is characterized by new muscle weakness, fatigue, and pain in polio survivors decades after their initial bout of polio. It is believed to be caused by overwork of motor neurons that survived the initial poliovirus infection but were left vulnerable. As time passes, these neurons fatigue and can no longer sufficiently innervate muscles. Treatment focuses on managing new symptoms, preserving function through exercise and assistive devices, and addressing pain. Physiotherapy plays a key role through energy conservation techniques, strengthening, and physical modalities like heat.