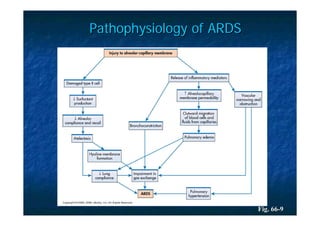
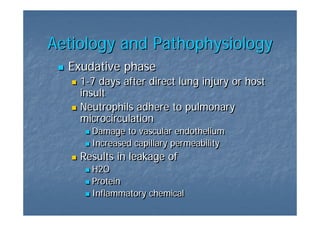
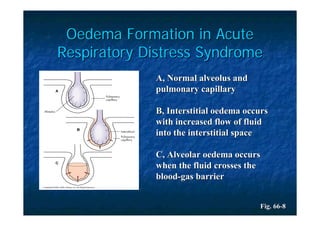
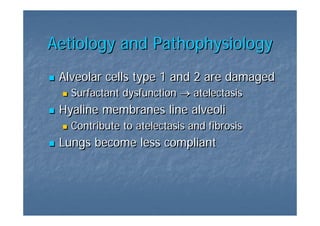
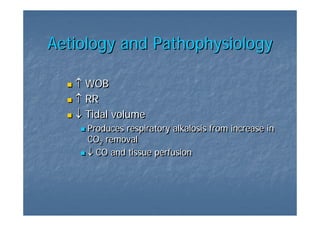
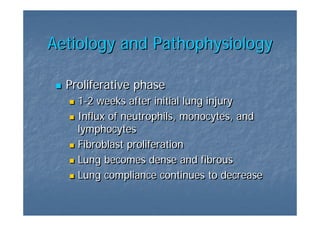
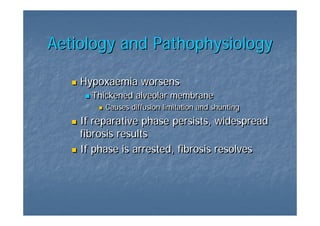
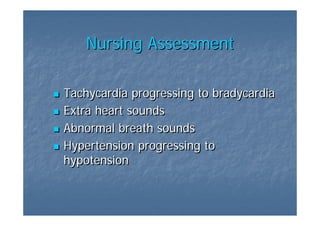
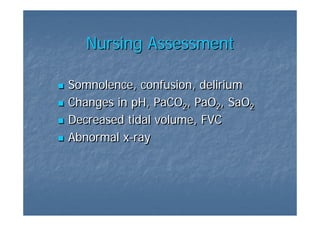
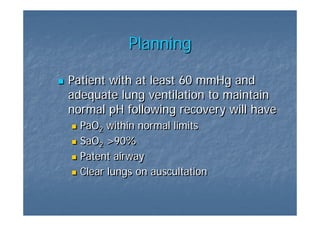
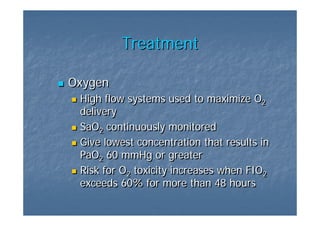
Acute Respiratory Distress Syndrome (ARDS) is a sudden, progressive form of respiratory failure characterized by severe dyspnea, hypoxemia, and decreased lung compliance. It develops from direct or indirect lung injuries and is thought to be caused by stimulation of the inflammatory and immune systems, resulting in leakage of fluid into the lungs. The clinical progression of ARDS involves exudative, proliferative, and fibrotic phases that can lead to respiratory failure if not promptly treated with oxygen supplementation, mechanical ventilation, and other supportive therapies.