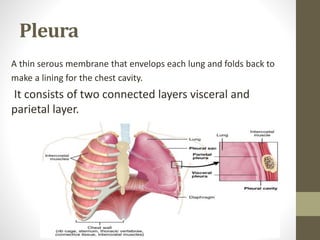
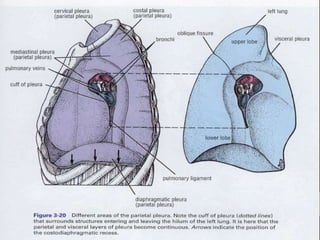
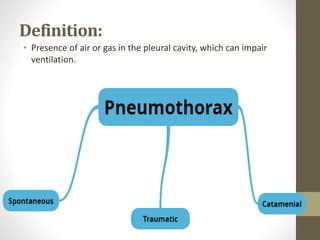
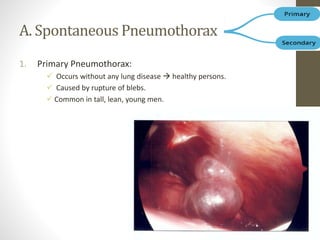
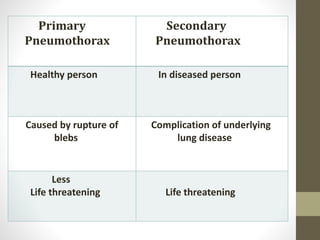
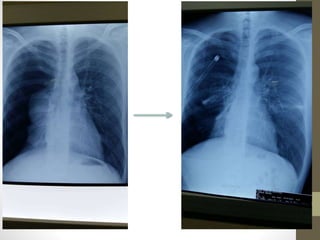
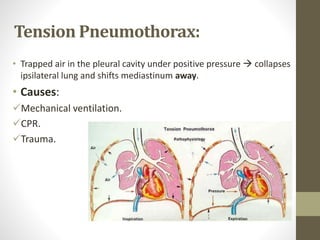
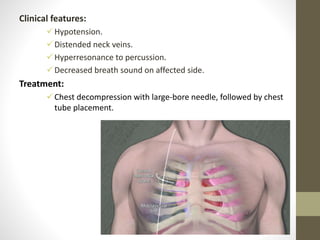
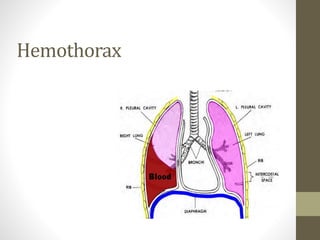
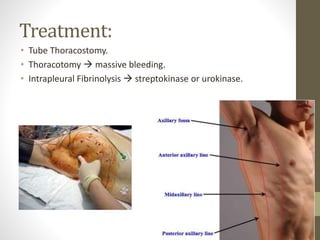
The document discusses anatomy and physiology of the pleura. It describes the two layers of pleura - parietal and visceral layers. The parietal layer lines the chest wall and diaphragm. The visceral layer covers the lungs. Between the two layers is a potential space that normally contains a small amount of fluid. The document also discusses intrapleural pressure, intra-alveolar pressure, and transpulmonary pressure. Pleural effusions, pneumothorax, and hemothorax are also summarized.