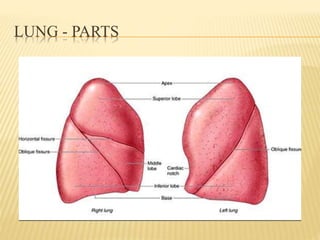
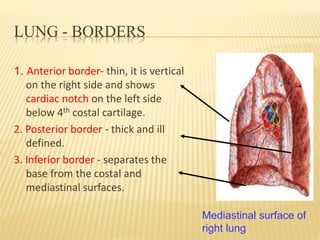
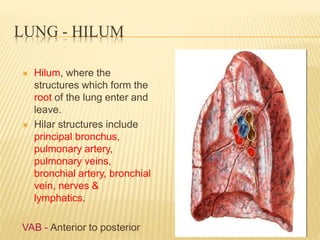
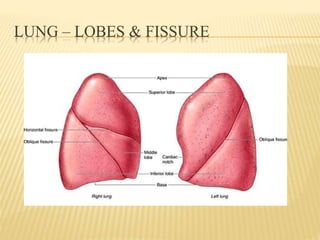
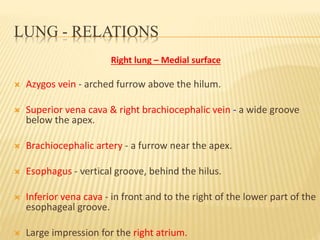
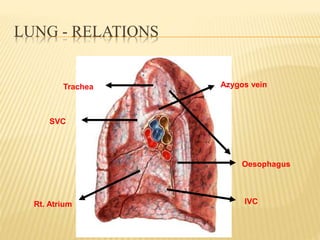
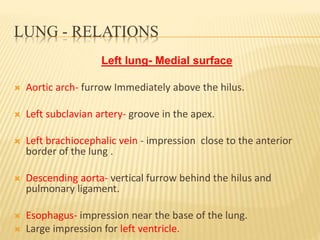
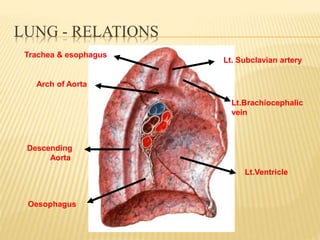
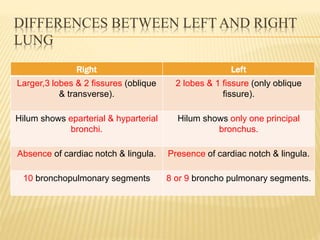
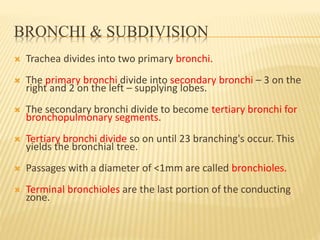
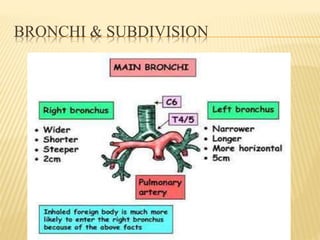
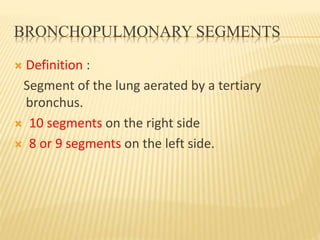
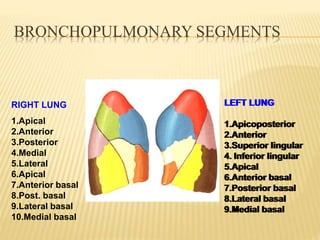
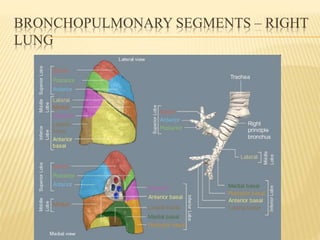
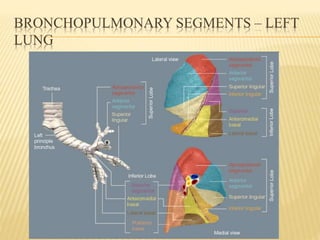
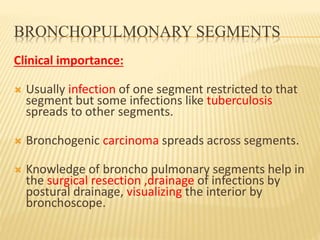
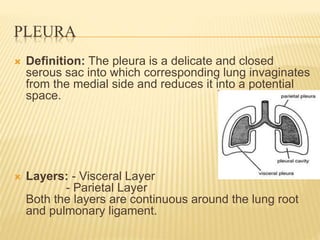
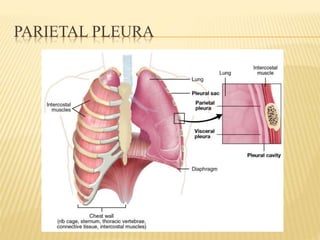
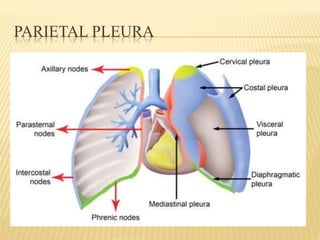
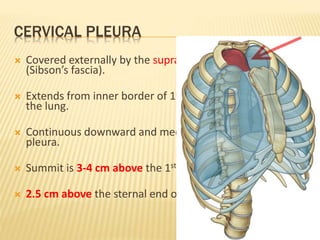
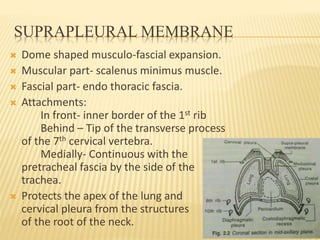
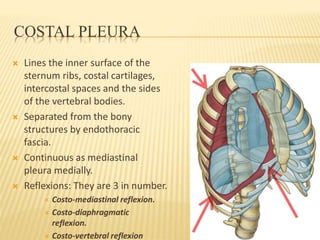
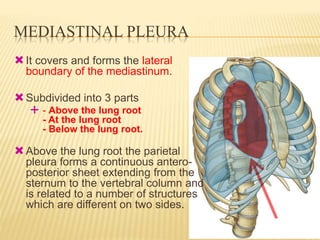
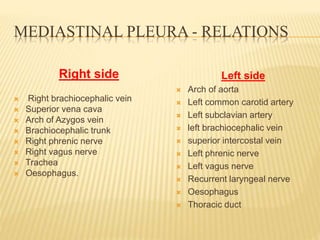
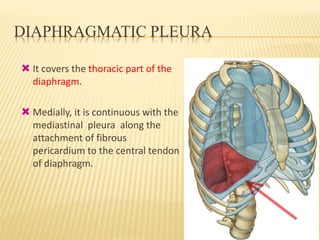
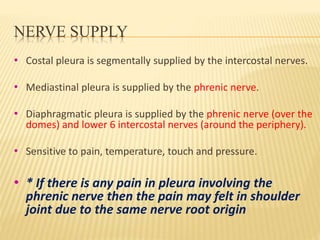
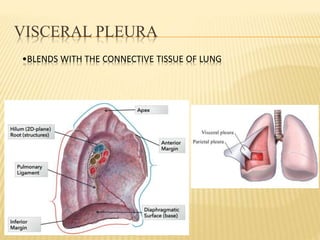
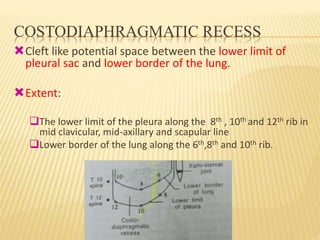
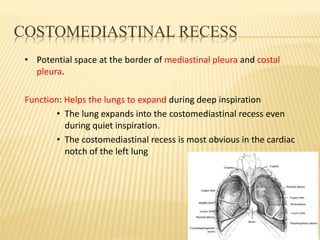
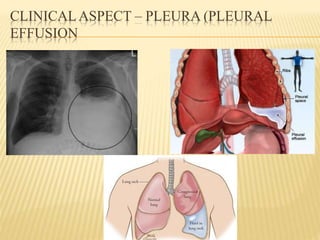
This document provides an overview of the pleura and lung. It begins by introducing the lung and its parts, including lobes and borders. It then describes the pleural layers in detail, including the parietal pleura layers of cervical, costal, mediastinal and diaphragmatic pleura. Relations and blood supply of the pleura are discussed. Bronchopulmonary segments and clinical significance are summarized. Common pleural conditions like pleurisy, pleural effusion and pneumothorax are briefly mentioned.