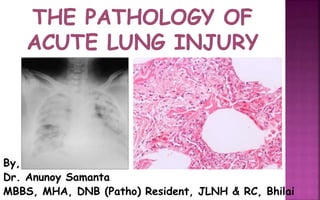
The Pathology of Acute Lung Injury
- 1. By, Dr. Anunoy Samanta MBBS, MHA, DNB (Patho) Resident, JLNH & RC, Bhilai
- 2. 1) Definitions of ALI/ARDS 2) Epidemiology 3) Etiology 4) Risk Factors for ARDS 5) Pathophysiology 6) Three Phases 7) Clinical Features 8) Clinical Diagnosis 9) Radiological Diagnosis 10) Biomarkers 11) Pathological Diagnosis 12) Are Pathologists Needed? 13) Gross Appearance 14) Histologic Patterns 15) Findings in COVID-19 16) Approach to a Lung Bx specimen 17) Summary
- 3. Acute Lung Injury (ALI) refers to a stereotypical pattern of lung injury, secondary to a wide range of pulmonary & extra-pulmonary insults, encompassing a continuum of clinical & radiographic changes that affect the lungs, with Acute Respiratory Distress Syndrome (ARDS) representing the severe end of this continuum. It’s too generalized. Clinicians need a working definition!
- 4. In 1915, although the terms ALI/ARDS weren’t used per se, a physician serving with the Canadian Forces, described the condition of a soldier’s lungs exposed to poison gas as “Shock Lung”. In 1967, Ashbaugh and colleagues coined the term ARDS to describe a clinical syndrome characterized by “an acute onset of tachypnea, hypoxemia and loss of compliance after a variety of stimuli”. In 1994, after decades of confusion with myriad definitions, finally the American-European Consensus Conferences (AECC) on ARDS recommended the adoption of an acceptable definition for ALI/ARDS.
- 5. Acute onset of diffuse, B/L pulmonary infiltrates documented by CXR, consistent with pulmonary edema. PaO2:FiO2 <= 300 (for ALI) & <=200 (for ARDS) PAWP <= 18 mm of Hg, or no clinical evidence of cardiac failure/ left atrial hypertension. This 3 criteria definition by AECC was clinically relevant, easy to use & capable of quantifying the severity of lung injury. Thus, it was ideal for use both in the clinical setting & for research purposes.
- 6. The radiological criteria are nonspecific & subject to inter-observer variability. ‘Acute’ was ill defined. There was no standard ventilation protocol for patients before meeting the criteria for hypoxemia. E.g. PaO2:FiO2 can simply be raised by increasing PEEP. PAWP may oscillate above & below cut-off. It can also be elevated for reasons other than heart failure.
- 7. According to the Berlin definition framed by a panel of experts in 2012, ARDS is an acute diffuse, inflammatory lung injury, leading to increased pulmonary vascular permeability, increased lung weight, and loss of aerated lung tissue, with hypoxemia, & B/L radiographic opacities associated with increased venous admixture, increased physiological dead space & decreased lung compliance. It categorized ARDS (on PEEP >= 5 cm of H2O) as:- Mild: 200 < PaO2:FiO2 <= 300 Moderate: 100 < PaO2:FiO2 <= 200 Severe: PaO2:FiO2 <= 100
- 8. Acute- means onset <= 1 week B/L opacities consistent with pulmonary edema must be present & may be detected on CT (thorax) or CXR PaO2:FiO2 <= 300 with a minimum of 5 cm H2O PEEP “must not be fully explained by cardiac failure or fluid overload,” in the physician’s best estimation using available information. An objective assessment (e.g. Echocardiogram) should be performed in most cases in the absence of a clear cause such as trauma or sepsis.
- 9. Berlin definition doesn’t include underlying aetiology & lacked a direct measure of lung injury. It doesn’t allow early identification of patients who may be amendable to therapies before establishment of ARDS. It still allows CXR to be used for diagnosis which compares poorly with CT (thorax). It has low sensitivity (True Positivity Rate) when compared to autopsy findings (~ 89%). Although slightly better than AECC, its ability to predict mortality is still poor.
- 11. Berlin definition, although widely in practice, is not suitable in resource-constrained settings with difficult access to arterial blood gas data, CXR & mechanical ventilation. In 2015, Riviello & colleagues developed a modification of the Berlin criteria to define ARDS & called it Kigali modification. It differed in:- No minimum PEEP requirement SpO2:FiO2 <= 315 B/L chest opacities evaluated by using of USG: B Lines or lung consolidation without pleural effusion in at least one field on each side of the chest is considered to be consistent with B/L lung opacities. CXR done when available.
- 13. Occur in all age groups. Mean age is 60 years. Male : Female = 3:2 Incidence 15-30 per 1,00,000 person/year Incidence of ARDS in ICU: - 10.4% of all ICU patients - 67.2% of all patients with acute hypoxemic respiratory failure - ARDS is frequently undiagnosed or late diagnosed Mortality- 30-40% for past 2 decades ARDS : ALI = 70% Not all ARDS show DAD (diffuse alveolar damage) pattern (58% in open lung Bx Vs 45% in autopsy findings)
- 14. ALI is a multi-factorial disease process that occurs due to an environmental trigger on the background of a genetic predisposition. The most common cause of ALI in our country is pneumonia, whereas in UK, sepsis accounts for the majority of case load. Although genetic markers have been identified that are associated with a phenotype that predisposes to ALI, the exact genetic basis of ALI still remains elusive due to:- (i) diversity in environmental stimuli involved, (ii) the complex gene-environment interaction, (iii) the heterogeneous nature of the disease itself & (iv) the presence of myriad co-morbidities.
- 16. We classify these causes as direct or indirect depending on the mechanism of injury to the lung:- (i) Direct / Pulmonary Causes: Infectious Pneumonia- Bacteria (Mycoplasma, Mycobacteria, Legionnela, Rickettsia), Virus ( Influenza, Herpes, CMV, Hanta, COVID-19), Fungi (Pneumocystis jirovecii) Aspiration of gastric contents Inhalation injury (Smoke, SO2, NO2) Near drowning Fat emboli Pulmonary contusion
- 17. (ii) Indirect / Extra-Pulmonary Causes: Sepsis (Pseudomonas Sp, E. coli, Staph aureus) Severe trauma/burn especially with shock & multiple transfusions. Drug (MTX, AZA, Bleomycin, Amiodarone, Gold, Penicillamine, Nitrofurantoin) Autoimmune diseases (Amyopathic dermatomyositis, SLE, RA, Scleroderma, Polyarteritis nodosa) Acute Pancreatitis Cardio-pulmonary bypass
- 18. Increased severity and extent of illness as measured by Injury Severity Score (ISS) or APACHE Score.
- 19. Patients with ALI progress through a similar patho- physiological process irrespective of whether the damage is a direct effect on the alveolar epithelial cells by an external stimulus or an indirect process resulting from a more distant systemic inflammatory process mediated via cytokines:-
- 23. ALI is a consequence of alveolar injury which produces diffuse alveolar damage (DAD). The injury causes the release of pro- inflammatory cytokines. Cytokines recruit neutrophils to the lungs where they get activated & release toxic mediators that damage the capillary endothelium & alveolar epithelium
- 24. In healthy lungs, there is a small amount of fluid that leaks into the interstitium. Our lymphatic system removes that fluid & returns it into the circulation, maintaining the alveoli dry.
- 26. Damage to the capillary endothelium and alveolar epithelium allows protein to escape from the vascular space!
- 27. Now, the oncotic gradient that allows resorption of fluid is lost & fluid pours into the interstitium, overwhelming the lymphatic system.
- 28. Breakdown of the alveolar epithelial barrier allows the air spaces to fill with bloody, proteinaceous edema fluids & debris from degenerating cells. Functional surfactant is lost resulting in alveolar collapse!
- 29. Healthy lungs can regulate the movement of fluid to maintain a small amount of interstitial fluid and dry alveoli. But, lung injury interrupts this balance, causing excess fluid in both the interstitium & alveoli. This excess fluid results in:- Impaired gas exchange Decreased compliance Increased pulmonary arterial pressure
- 32. (1) Acute/Early/Exudative Phase (4-7 days):- Alveolar Changes: - Hyaline membrane on alveolar duct or sacs - Interstitial & intra-alveolar edema - Collapsed alveoli Epithelial Changes: Denudation & necrosis of Type I pneumocytes Vascular Changes: - Necrosis of endothelial cells - Neutrophil aggregation - Micro thromboembolism - Hemorrhage
- 33. Acute exudative phase of DAD showing prominent hyaline membranes Interstitial edema & inflammation are present Alveolus contains edema fluid as well as a number of inflammatory cells including RBCs.
- 34. (2) Proliferative/Organizing Phase (>7 to 21 days):- Alveolar Changes: - Organizing or remnants of hyaline membrane - Interstitial & intra-alveolar proliferation of fibroblasts /myofibroblasts - Lymphocytic infiltration Epithelial Change: Proliferation of Type II pneumocyte Vascular Changes: - Endothelial injury - Thromboembolism in arteries & arterioles
- 35. The alveolar walls are markedly expanded by extensive fibroblastic proliferation, accompanied by mild inflammation & edema Remnants of hyaline membranes are seen Thrombus seen in an arteriole
- 36. Micrographs of proliferative phase highlighting Type II pneumocyte hyperplasia
- 37. Micrograph of late proliferative phase with extensive interstitial & intra-alveolar fibroblastic proliferation
- 38. (3) Resolving/Fibrotic Phase (>21 days):- Alveolar Changes: - Diffuse collagenous fibrosis - Microscopic honeycomb like change - Traction bronchiolectasis Epithelial Change: Squamous cell hyperplasia Vascular Changes: - Remodelling of arteries - Fibrosis in intima - Thickening of media
- 39. Fibrotic phase of DAD showing collapsed/enlarged alveoli along with Squamous metaplasia
- 40. (1) Acute Phase:- Acute & progressive Respiratory Failure: Usually starts 12-48 hrs after the initial insult, dyspnoea on exertion followed by dyspnoea at rest Hypoxemia resistant to O2 therapy: PaO2:FiO2 <= 300 Diffuse, fine crepitations on auscultation Often accompanied by signs of sepsis and MODS! (2) Organizing Phase:- Resolution of hypoxemia Improved lung compliance (3) Fibrotic Phase:- Continued hypoxemia Decreased pulmonary compliance & Right heart failure
- 41. ALI/ARDS is typically a diagnosis based on clinical & radiological features, with DAD being the histological counterpart only . Presently we’re using well defined clinical criteria as proposed in Berlin definition, with a keen focus on ABG analysis.
- 42. Geographic distribution of patchy ground-glass densities & areas of lobular sparing are radiologic hallmark of Chest X- Ray in ALI/ARDS. Acute phase shows B/L whiteout appearance with patchy consolidations Fibrotic phase may show interstitial appearance.
- 43. Most common CT (thorax) findings are:- B/L, basilar (68%), patchy (42%), predominantly dependent (86%) abnormalities Areas of consolidation & air bronchograms (89%) Details of the disease status can be best studied around the areas of consolidation & fibrosis
- 45. Bronchoscopic Lavage (BAL) sample if obtained usually shows:- Cytology- Reactive epithelial cells, alveolar macrophages and neutrophils Giemsa, ZN Staining might identify the specific organism
- 46. BAL of a patient with ARDS who tested + for COVID19 shows: Reactive broncho-epithelial cells with non-specific viral like nuclear & cytoplasmic changes in a background of severe acute inflammation.
- 47. DAD is the main pattern of lung injury. Ironically most of our findings are AUTOPSY BASED only. Biopsies (Wedge Bx) are seldom sought for in the diagnosis, when:- Presentation isn’t straightforward Specific infection is being suspected Therapeutic response is poor Autopsy cases
- 48. Patel et al (2004): In selected patients with clinical ARDS, open lung Bx (OLB) can be performed safely, often reveals an unsuspected Dx, & frequently leads to alterations in therapy. Alexandra K. Et al (2015): Among mechanically ventilated patients with respiratory failure of unclear etiology, lung Bx yielded a wide range of Dx & was associated with change in therapy in most patients. Carole et al (2018): OLB can play an useful role in the Mx of ICU patients with ARF of undetermined origin, including ARDS mimickers. Gerard et al (2018): OLB was able to identify a steroid-sensitive pathology in a significant proportion of non resolving ARDS patients. These patients had a better outcome with lower hospital mortality.
- 49. All these studies clear our doubts. Yes, PATHOLOGISTS ARE NEEDED in managing ALI/ARDS cases too! Pathologists can help in the:- Evaluation of a specific infectious cause Correlation with clinical findings, and thus understanding the pathogenesis better, which in turn shall aid in the evolution of new targeted therapies Increasing sensitivity of the chest radiograph so that steroids could be added at the beginning of the fibrotic process in ARDS.
- 50. Autopsy specimens of lungs usually are:- Dark blue lungs with dots of haemorrhage on pleural surface Heavy, firm due to edema & fibrosis Here we find diffuse consolidation of all lobes representing DAD
- 51. Diffuse Alveolar Damage (DAD) is the classic histo- pathological manifestation of ALI/ARDS & it has been discussed earlier in fair details. Here we’ll checkout the most important differentials of DAD:- Usual Interstitial Pneumonia (UIP) Non-specific Interstitial Pneumonia (NSIP) Cryptogenic Organizing Pneumonia (COP) Acute Eosinophilic Pneumonia (AEP) Acute Fibrinous & Organizing Pneumonia (AFOP) Diffuse Alveolar Haemorrhage (DAH) with capillaritis Organizing Pneumonia (OP)
- 52. Microscopic findings in UIP pattern:- Dense Fibrosis & Architectural Distortion Patchy & peripheral/ perilobular involvement Honeycomb appearance Fibroblastic foci
- 53. (a) OLB showing fibrotic lung dz with heterogeneous spatial & temporal fibrosis consistent with UIP pattern. (b) Honeycomb change with enlarged subpleural alveolar spaces, with bronchiolar metaplasia, mucus plugs & mild chronic inflammatory infiltrates are visible in the section studied
- 54. Microscopic findings in NSIP pattern:- Diffuse & uniform inflammation (on low power) of alveolar wall, bronchovascular bundles & pleura. Lymphocytic or plasmacytic infiltration Loose fibrosis Lung architecture frequently preserved
- 55. (A) Uniform & diffuse thickening of the alveolar walls in NSIP (B) Alveolar septa thickened by the inflammatory cell infiltrate & mild interstitial fibrosis, without remodelling the basic lung structure
- 56. Microscopic findings in COP pattern:- OP- Fibroblastic plugs in alveolar sacs, ducts & bronchiolar lumen Mild to moderate cellular infiltrate Alveolar architecture usually preserved Foamy macrophages in surrounding airspace may be present
- 57. (A) Involvement is often patchy & the border between COP & normal lung is relatively clear (B) The basic lung architecture is maintained (C,D) The polypoid organization is composed of myofibroblasts.
- 58. Microscopic findings in AEP pattern:- Alveolar & interstitial infiltration by eosinophils, plasma cells & histiocytes Variable angitis, fibrosis, mucus plugging & bronchiolitis with necrosis May have Charcot- Leyden crystals
- 59. (A) Many eosinophils are visible in air spaces in a patient of AEP (B) Organization in alveolar spaces seen. Hyaline membrane are rarely present
- 60. Microscopic findings in AFOP pattern:- Intra-alveolar fibrin called “fibrin ball” OP- Fibroblastic plugs in alveolar sacs & ducts with loose collagen matrix Diffuse & patchy distribution Lymphoplasmacytic infiltrate
- 61. (1) “Fibrin balls” without formation of hyaline membranes (2) Intra-alveolar fibrin & OP with patchy involvement (3) AFOP with diffuse involvement (4) Fibroblastic tissue surrounding alveolar fibrin
- 62. Microscopic findings in DAH with capillaritis:- Diffuse, intra-alveolar blood admixed with hemosiderin laden macrophages with coarsely granular & golden brown pigment Significant neutrophilic infiltrates within alveolar septae with vascular necrosis Hyaline membrane present Fibroblastic tissue forming ‘dumbbell’ shapes
- 63. Capillaritis in DAH is distinctive but can be quite focal in a Bx specimen. The section shows variable fresh blood in the parenchyma, typically associated with fibrin, reactive Type II cells & haemosiderin laden alveolar macrophages
- 64. Microscopic findings in Organizing Pneumonia (OP) pattern:- Exudate of fibrin & neutrophils transforming into fibromyxoid masses with histiocytes May have necrotizing changes in the bronchi We’ve already observed this beautiful pattern while discussing AFOP, DAH with capillaritis & COP
- 66. * Based on minimally invasive autopsy:- Pulmonary changes in the form of DAD Multinucleated enlarged pneumocytes with large nuclei, amphophilic cytoplasm & prominent nucleoli in alveolar spaces Intranuclear inclusions May be superimposed by bacterial pneumonia * BAL Cytology:- Abundant activated plasma cells Alveolar macrophages may feature nuclear clearing or intranuclear cytopathic inclusions
- 67. COVID-19 + Case: (A) Proteinaceous exudates in alveolar spaces with granules; (B) Scattered large protein globules; (C) Intra-alveolar fibrin with early organization, mononuclear inflammatory cells & multinucleated giant cells; (D) Hyperplastic pneumocytes, some with possible viral inclusions.
- 68. COVID-19 + BAL: (A) Many clusters of activated plasma cells; (B) Alveolar macrophage intranuclear cytopathic inclusion; (C,D) Groups of polyclonal CD-138 + plasma cells.
- 70. Coordinate with clinician colleague & extract maximum Clinical information: relating disease onset, progression, suspected underlying etiologies, radiographic findings, whether the patient is on mechanical ventilation etc Careful evaluation for potential infective etiologies should be done in every case: Special stains for microorganisms namely an Acid-fast stain, a Grocott- Gomori-methenamine-silver (GMS) & a bacterial stain such as Brown-Hopps should be obtained, & should be meticulously scrutinized for viral cytopathic changes. Although a wedge Bx is recommended, as a pathologist we usually end up receiving small Bx specimens especially in the initial stages of the clinical workup. A precise Dx may not be possible in many cases.
- 71. In this case of AFOP, numerous fungal organisms, compatible with Aspergillus were present. These organisms were not visible on the H&E section (B), but could be easily appreciated on staining with Gomori-methenamine-silver.
- 72. Gomori-methenamine-silver stain showing:- 1) Pneumocystis carinii and 2) Cryptococcus neoformans respectively
- 73. 1) Brown-Hopps stain showing E. coli 2) Z-N stain showing M. tuberculosis
- 74. * Hyaline membrane may not be detectable. We’ve to still check for the presence of:- Intra-alveolar edema/Myxoid interstitial fibrosis Marked pneumocyte hyperplasia with bizarre cytologic features Alveolar fibrin/debris * If these (or any of these) features are appreciated in a patient with known respiratory failure, it’s best to:- Provide a descriptive Dx with a comment that the findings are suggestive of, or consistent with ALI Avoid over-interpretation of findings & be conservative when correlative information is unavailable
- 75. This small Bx section showing intra-alveolar fibrin with mild expansion of the alveolar septa & pneumocyte hyperplasia. These findings aren’t specific per se. But, when applied on a patient with diffuse pulmonary infiltrates & respiratory compromise, it can be reported to be consistent with ALI
- 76. When a diagnosis of ALI is suspected we must evalute for the presence of:- * Microorganisms and viral inclusions * Eosinophils (suggesting the possibility of AEP) * Coarse hemosiderin & capillaritis (suggesting an immune mediated vasculitis DAH) Be mindful of the presence of fresh haemorrhage secondary to Bx procedure. Blood & associated fibrin in air spaces shouldn’t be over-interpreted as hyaline membrane. Here the fibrin would be loose & wispy. Procedure-related haemorrhage unless supported by macrophages with coarse hemosiderin granules or reactive pneumocytes shouldn’t be over- interpreted as DAH.
- 77. Hemosiderin secondary to alveolar haemorrhage typically consists of large coarse granules (A), in contrast to the finely granular pigment (B) associated with cigarette smoking.
- 78. (A) Neutrophilic capillaritis is characterized by prominent PMNs within the alveolar septa. Neutrophilic debris or fibrin thrombi suggests underlying vascular damage. (B) Healing capillaritis is characterized by organizing fibroblastic tissue. Often the organizing tissue bridges the previously damaged alveolar septa in a ‘dumbbell’ fashion.
- 79. ALI/ARDS clinically represent a significant cause of pulmonary morbidity & mortality. Majority of patients with these conditions will have a histologic pattern of DAD, but not all. So, conditions like AFOP, AEP, UIP, NSIP, COP, DAH with capillaritis may also be encountered which comprise genuine consideration for the differential diagnosis. Determination of potential infective etiologies is important from the pathologist’s perspective, and due caution should be exercised in interpreting small Bx specimens.
