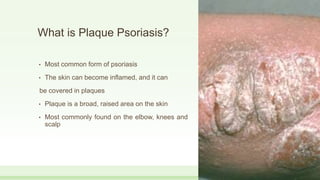
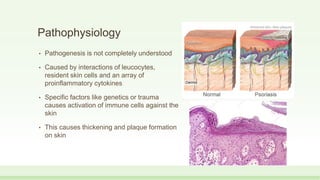
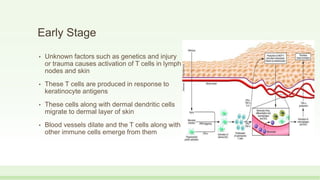
Plaque psoriasis is the most common form of psoriasis, characterized by raised, inflamed patches of skin covered in silvery scales. It is caused by an immune system dysfunction that causes skin cells to grow too quickly. Risk factors include family history, stress, obesity, and smoking. Diagnosis is usually made through physical exam, and treatments include topical creams and ointments, light therapy, and systemic medications depending on severity.

![• Light therapy [Photo therapy]
the treatment uses natural sunlight or artificial UV
light.
• They include ……..
• Sunlight
• exposure to UV light slows down skin growth
reducing scaling and inflammation.
• exposure to sunlight everyday may improve skin.
• But intense exposure to sunlight may worsen the
condition.](https://image.slidesharecdn.com/plaquepsoriasispresentation-190319013729/85/Plaque-psoriasis-presentation-36-320.jpg)