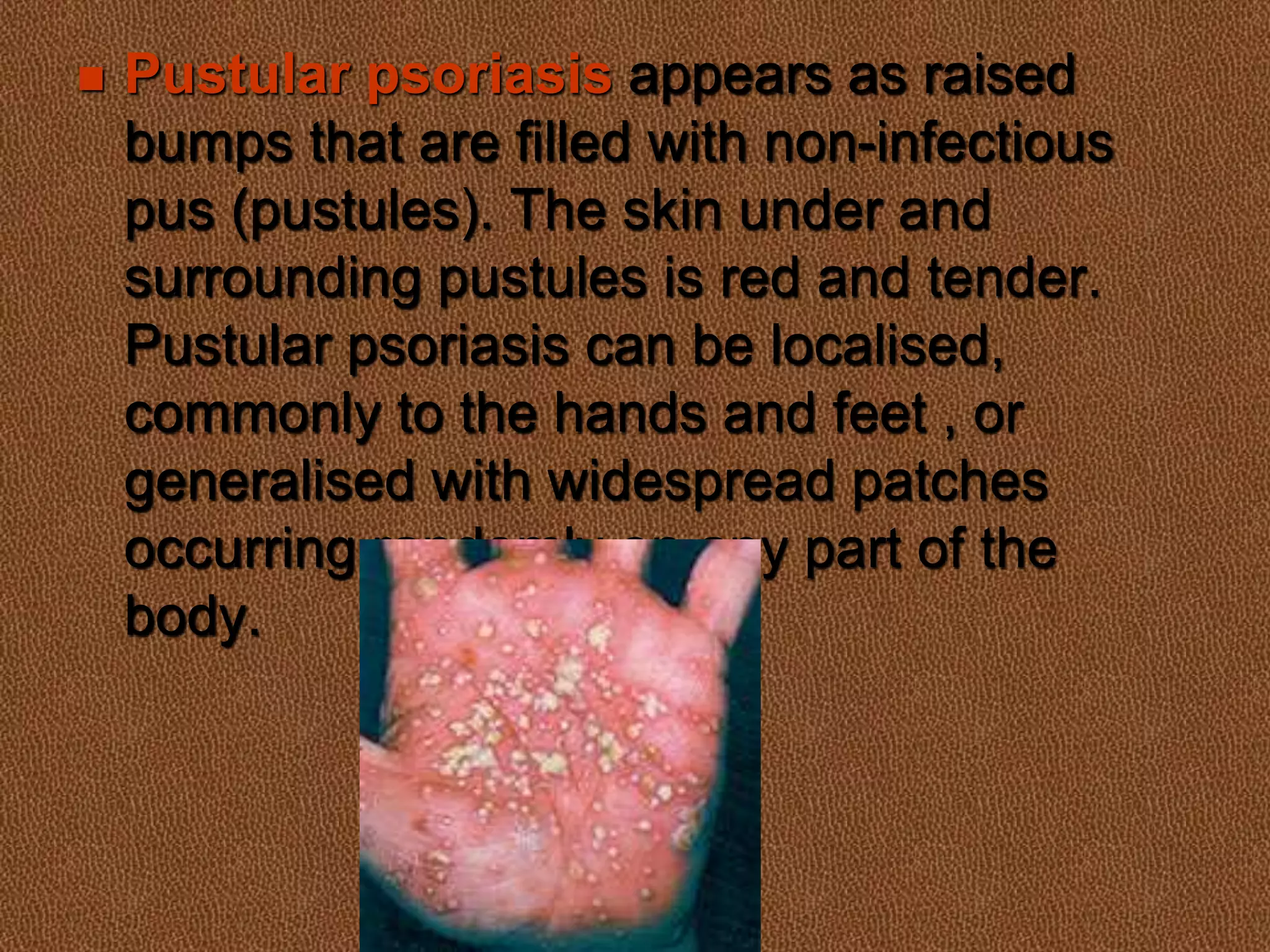
Psoriasis is a chronic inflammatory skin disease characterized by rapid skin cell production, leading to red, scaly patches called plaques, which can occur anywhere on the body and may involve joint inflammation known as psoriatic arthritis. The condition varies in severity and is influenced by genetic factors and potential triggers such as stress and alcohol consumption. While there is no cure, treatments including topical applications, phototherapy, and systemic medications can help manage symptoms, but risks of significant morbidity are associated with some treatments.